Ideas on my blog has evolved as more and more information have become available. This post is an attempt to bring readers up to date with my current thinking. I am striving to be transparent in my logic -- showing the evidence that I am working off and my thought process.
Microbiome Definition of CFS/FM/IBS
A condition that results from:
Replace the metabolites produced by the missing bacteria
Replacing the metabolites should result in the reduction of symptoms associated with a deficiency of these metabolites.
See this post for the study references. These items should/could be done continuously.
The items below were found in studies to increase bifidobacterium and lactobacillus:
Bootstrapping E.Coli
The E.Coli probiotics below are human sourced and known to take up residency in the human gut.
The other microbiome shifts appear to be in different clusters of microbiome shifts. The 2017 paper by Peterson, Klimas, Komaroff, Lipkin (and a stack of other CFS researchers) makes that clear in it's title: "Fecal metagenomic profiles in subgroups of patients with myalgic encephalomyelitis/chronic fatigue syndrome"
The best way at present to proceed is to get uBiome.com done.[No financial interest]. When the results come in, click on the Compare tab, then go to Genus, click on ratio twice so the results are in descending order.
This is the "hit list" of what you are trying to reduce. DataPunk.Net provides a nice summary of what we know about these. For example, Alistipes: https://www.datapunk.net/substrata/display.pl?239759+S

At this point, we hit a cognitive challenge. You want to avoid items that are "Enhanced By" which is in common across all of the high items, take the items that are "Inhibited By" which are NOT on any of the "Enhanced By" lists. You may also wish to reduce foods that are high in items listed in "Nutrients/Substrates". It becomes a jig-saw puzzle! I have done this exercise for some uBiome.
Some of these items are contraindicated with a few uBiomes that I have reviewed. This likely is why person B reports no results while person A reports improvement. Example: Magnesium is usually very helpful -- but there are a few cases where it encourages overgrowth of undesired bacteria.
Probiotics
Most probiotics do not take up residency, "here today, gone tomorrow". Their primary role in my model is producing natural antibiotics against other bacteria. An example:
Why 3x per day? Simple: because almost none of them are detected after 12-24 hrs... so to keep them (and the production of natural antibiotics going) you need to keep taking them during the day. See this post for citations.
The following appears to actually help. Some probiotics may make your symptoms worst! Unfortunately, most commercial probiotics contains some of those.
Teas
Some teas can also be antibiotics (among other roles). There are two teas that seem to produce significant results quickly:
Herbs and Spices
The best choice needs examination of your microbiome (i.e. uBiome results) and doing the work cited above. Survey results found:
If you do not know your microbiome, then see https://cfsremission.com/reader-surveys-of-probiotics-herbs-etc/ for suggestions. Your results will vary because your microbiome vary.
Thick blood is an issue also -- but here things gets more complicated and not suitable for this recap.
Antibiotics can have a role -- but getting prescriptions for the right ones can be a major challenge.
Bottom Line
Working with the microbiome and autoimmune is like working with fragments of the dead sea scrolls. For many bacteria we can identify it -- what inhibits or encourages it is not known to modern medical science. We have extremely thin slices of knowledge --Almonds Bifidobacterium, Lactobacillus (B&L) as do sesame seeds. What about sunflower seeds? Peanuts? Cashews? We find that Walnuts help the bacteria that inhibits B&L -- so we cannot safely generalize to "all seeds/nuts are helpful".
In many cases, we find that healthy diet or supplements demonstrated to work for normal people have the opposite effect on CFS and other altered microbiome conditions. This is made even worst because most of the studies were done on males and most people with CFS are females. We end up having to swim up-stream thru good and valid suggestions -- that are just wrong for us.
My model is simple to understand and allows us to filter many suggestions and candidates. With the availability of uBiome testing (without needing a prescription!) we have entered the age of explicit treatment based on your unique microbiome. We do not know the role of many bacteria involved. We do not know what will inhibit or enhanced all of these bacteria. Frustrating little knowledge!
On the flip side, many readers have reported significant improvement, reduction of prescription medication, etc. so the model and suggestions have potential and thus hope of remission! Microbiome studies are exploding on PubMed, a lot of research is being done and we can often borrow their results.
This is an education post to facilitate discussing this approach with your medical professionals. It is not medical advice for the treatment of CFS. Always consult with your medical professional before doing any changes of diet, supplements or activity. Some items cites may interfere with prescription medicines.
Microbiome Definition of CFS/FM/IBS
A condition that results from:
- Low or no Lactobacillus
- Low or no Bifidobacteria
- Low or no E.Coli
- A marked increase in number of bacteria genus (as measured by uBiome) to the top range
- Most of these genus are hostile to/surppress Lactobacillus, Bifidobacteria, E.Coli
- Several are two or more times higher than normally seen
- The number of bacteria genus goes very high (using uBiome results), but most of them are low amounts.
("Death by a thousand microbiome cuts" and not "Death by a single bacteria blow")
- The appearance of rarely seen bacteria genus in uBiome Samples.
Replace the metabolites produced by the missing bacteria
Replacing the metabolites should result in the reduction of symptoms associated with a deficiency of these metabolites.
See this post for the study references. These items should/could be done continuously.
- Acetylcholine See this post
- Warning: lots of writing on the web. Some suggestions are contraproductive.
- Regular eating of almonds
- Repeated administration of almonds increases brain acetylcholine levels and enhances memory function in healthy rats while attenuates memory deficits in animal model of amnesia [2016].
- Riboflavin (B2) [1999]
- 400 mg/day [Src]
- Biotin (B7)
- 100 mcg/day [Src]
- Folate (B9)
- 6,000 mcg and 13,000 mcg of Folate, OR
- 15 mg of Folininc Acid [src]
- Vitamin B12
- 1000 mcg/ 1 mg [post]
- GABA
- 1000-3000 mg often cites on various sites
- Up to 0.8g/kg day [Src]
- Urolithins requires bacteria and dietary ellagic acid (pomegranate juice is a source).
- Bifidobacterium probiotics should be taken (at same time) WITH pomegranate juice.
- While the bifido will not stay around, they may utilize the pomegranate during their transit in your body)
- No dosage information.
- Bifidobacterium probiotics should be taken (at same time) WITH pomegranate juice.
- Vitamin D3 -15,000 IU/day
- "Baseline vitamin D level was found to moderate treatment effect on several outcome measures. Dry mouth and sleep disruption were reported more frequently in the placebo group. [Control took Lactobacillus helveticus and Bifidobacterium longum]" [2017]
- Vitamin D deficiency changes the intestinal microbiome reducing B vitamin production in the gut. The resulting lack of pantothenic acid adversely affects the immune system, producing a “pro-inflammatory” state associated with atherosclerosis and autoimmunity[2016].
- Thiamine Vitamin B1
- 100 mg 2 times a day
- Bacopa monniera and Cognitive Function
- Impacts GABA, acetylcholine
The items below were found in studies to increase bifidobacterium and lactobacillus:
- Bifidobacterium, Lactobacillus
- Sesame seed: Enhances Bifidobacterium Enterococcus Lactobacillus
- Dark Chocolate
Bootstrapping E.Coli
The E.Coli probiotics below are human sourced and known to take up residency in the human gut.
- Core: D-Ribose a preferred food that it uses
- Mutaflor probiotics -- E.Coli Nissle 1917
- Symbioflor 2 -- multiple strains
The other microbiome shifts appear to be in different clusters of microbiome shifts. The 2017 paper by Peterson, Klimas, Komaroff, Lipkin (and a stack of other CFS researchers) makes that clear in it's title: "Fecal metagenomic profiles in subgroups of patients with myalgic encephalomyelitis/chronic fatigue syndrome"
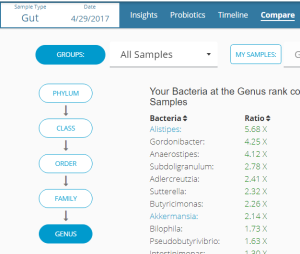
The best way at present to proceed is to get uBiome.com done.[No financial interest]. When the results come in, click on the Compare tab, then go to Genus, click on ratio twice so the results are in descending order.
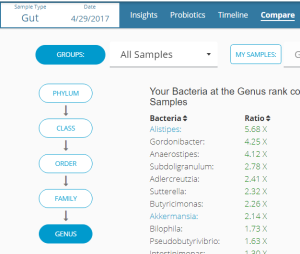
This is the "hit list" of what you are trying to reduce. DataPunk.Net provides a nice summary of what we know about these. For example, Alistipes: https://www.datapunk.net/substrata/display.pl?239759+S

At this point, we hit a cognitive challenge. You want to avoid items that are "Enhanced By" which is in common across all of the high items, take the items that are "Inhibited By" which are NOT on any of the "Enhanced By" lists. You may also wish to reduce foods that are high in items listed in "Nutrients/Substrates". It becomes a jig-saw puzzle! I have done this exercise for some uBiome.
- https://cfsremission.com/2017/09/11/ubiomes-before-and-after-a-fecal-microbiota-transplant/
- https://cfsremission.com/2017/09/03/ubiome-result/
- https://cfsremission.com/2017/09/18/another-ubiome-review-with-bifidobacteria-overgrowth/
- https://cfsremission.com/2017/08/27/ubiome-of-a-mcs-with-cfs-person/
- Alistipes: https://cfsremission.com/2017/10/09/decreasing-alistipes-genus/
- Anaerostipes: https://cfsremission.com/2017/10/07/decreasing-anaerostipes-genus/
- Clostridium https://cfsremission.com/2017/10/07/decreasing-clostridium-genus/
Some of these items are contraindicated with a few uBiomes that I have reviewed. This likely is why person B reports no results while person A reports improvement. Example: Magnesium is usually very helpful -- but there are a few cases where it encourages overgrowth of undesired bacteria.
Probiotics
Most probiotics do not take up residency, "here today, gone tomorrow". Their primary role in my model is producing natural antibiotics against other bacteria. An example:
- Inhibition of Clostridium perfringens by an antibiotic substance produced by Bacillus licheniformisin the digestive tract of gnotobiotic mice: effect on other bacteria from the digestive tract [1976].
- “Among those, seven Paenibacillus polymyxa strains showed the highest antibotulinal activity and the largest antimicrobial spectrum against C. botulinum strains. ” [2002] – this is in Prescript Assist Probiotics
Why 3x per day? Simple: because almost none of them are detected after 12-24 hrs... so to keep them (and the production of natural antibiotics going) you need to keep taking them during the day. See this post for citations.
The following appears to actually help. Some probiotics may make your symptoms worst! Unfortunately, most commercial probiotics contains some of those.
- Symbioflor-2
- Mutaflor
- Lactobacillus Fermentum ME3
- Lactobacillus Reuteri
- Lactobacillus Casei
- Bifidobacterium infantis
- Bifidobacterium Longum
- Bifidobacterium bifidum
- Bifidobacterium Breve
- Prescript Assist
- General Biotics Equilibrium
- ". The findings show that the six species of Bifidobacterium differed in their ability to relieve constipation. B. longum, B. infantis and B. bifidum were the most effective in relieving constipation, B. adolescentis and B. breve were partially effective and B. animalis was not effective. Furthermore, edible Bifidobacterium treated constipation by increasing the abundance of Lactobacillus and decreasing the abundance of Alistipes, Odoribacter and Clostridium. ." [2017]
Teas
Some teas can also be antibiotics (among other roles). There are two teas that seem to produce significant results quickly:
- Rosehip Tea
- Tulsi Tea
Herbs and Spices
The best choice needs examination of your microbiome (i.e. uBiome results) and doing the work cited above. Survey results found:
- Neem and Oregano with 80% improving
- Olive Leaf and Licorice with 56% improving
- Thyme with 50% improving
- Wormwood and Tulsi with 33% improving
If you do not know your microbiome, then see https://cfsremission.com/reader-surveys-of-probiotics-herbs-etc/ for suggestions. Your results will vary because your microbiome vary.
Thick blood is an issue also -- but here things gets more complicated and not suitable for this recap.
Antibiotics can have a role -- but getting prescriptions for the right ones can be a major challenge.
Bottom Line
Working with the microbiome and autoimmune is like working with fragments of the dead sea scrolls. For many bacteria we can identify it -- what inhibits or encourages it is not known to modern medical science. We have extremely thin slices of knowledge --Almonds Bifidobacterium, Lactobacillus (B&L) as do sesame seeds. What about sunflower seeds? Peanuts? Cashews? We find that Walnuts help the bacteria that inhibits B&L -- so we cannot safely generalize to "all seeds/nuts are helpful".
In many cases, we find that healthy diet or supplements demonstrated to work for normal people have the opposite effect on CFS and other altered microbiome conditions. This is made even worst because most of the studies were done on males and most people with CFS are females. We end up having to swim up-stream thru good and valid suggestions -- that are just wrong for us.
My model is simple to understand and allows us to filter many suggestions and candidates. With the availability of uBiome testing (without needing a prescription!) we have entered the age of explicit treatment based on your unique microbiome. We do not know the role of many bacteria involved. We do not know what will inhibit or enhanced all of these bacteria. Frustrating little knowledge!
On the flip side, many readers have reported significant improvement, reduction of prescription medication, etc. so the model and suggestions have potential and thus hope of remission! Microbiome studies are exploding on PubMed, a lot of research is being done and we can often borrow their results.
This is an education post to facilitate discussing this approach with your medical professionals. It is not medical advice for the treatment of CFS. Always consult with your medical professional before doing any changes of diet, supplements or activity. Some items cites may interfere with prescription medicines.
