A reader wrote:
“This week on our ABC National TV, the head of a big city hospital’s chronic fatigue clinic stated that there are no biological markers for chronic fatigue, so the best treatment was graded exercise and CBT. Unfortunately his opinion is very powerful here in patients getting government funding for help.”
See this link: http://www.abc.net.au/news/2018-07-18/chronic-fatigue-treatments-set-for-review/10007356
Beware of demanding a marker for all!
For most conditions there are multiple markers, if a significant number shows up — then conventional medical practice is to assume that condition. CFS traditionally require X out of Y symptoms that persisted for 6 months with all probable conditions accounting for those symptoms being excluded. It is unreasonable to expect every mixture of symptoms to have the same biological markers.
Statistically Significant Biological Markers against Control Populations
There are multiple markers. If a suspected CFS patient is tested for 2 (hereditary coagulation abnormality and SPECT scan), the odds of both being negative appears to be 3%.
Treatment is a different question — my focus has been on microbiome shifts. Several readers have reported major improvement with this approach — some returning to work (with some symptoms remaining). Fecal Matter Transplants have repeatedly resulted in short term remission — rarely lasted more than 6 months with several readers who have shared their experiences.
Microbiome shifts cannot be resolved with eating yogurt, kefir or even 99% of health food stores probiotics. There are overgrowths that need to reduced and undergrowths that need to be encouraged. At present, uBiome or thryve microbiome tests appear to be the best path forward — with end product production of the microbiome population appearing to be very significant for symptoms seen.
“This week on our ABC National TV, the head of a big city hospital’s chronic fatigue clinic stated that there are no biological markers for chronic fatigue, so the best treatment was graded exercise and CBT. Unfortunately his opinion is very powerful here in patients getting government funding for help.”
See this link: http://www.abc.net.au/news/2018-07-18/chronic-fatigue-treatments-set-for-review/10007356
Beware of demanding a marker for all!
For most conditions there are multiple markers, if a significant number shows up — then conventional medical practice is to assume that condition. CFS traditionally require X out of Y symptoms that persisted for 6 months with all probable conditions accounting for those symptoms being excluded. It is unreasonable to expect every mixture of symptoms to have the same biological markers.
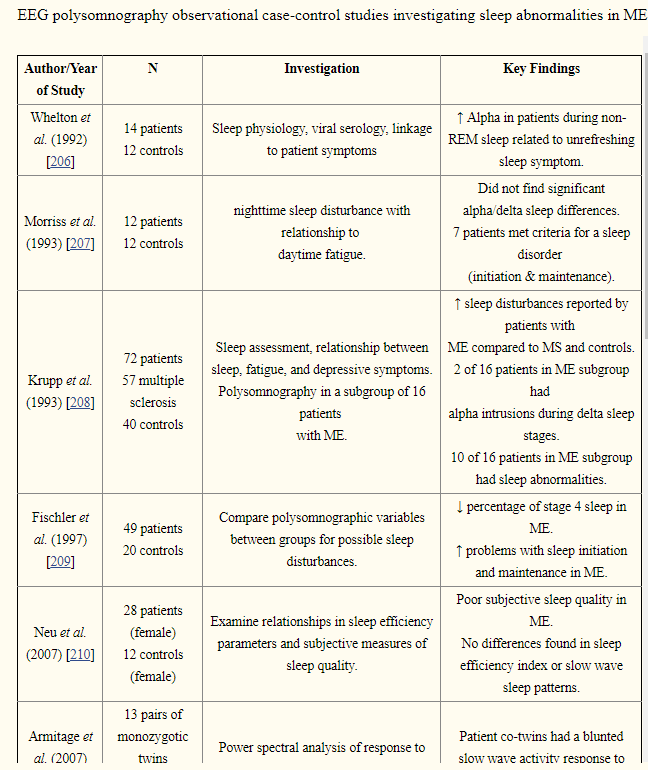
Statistically Significant Biological Markers against Control Populations
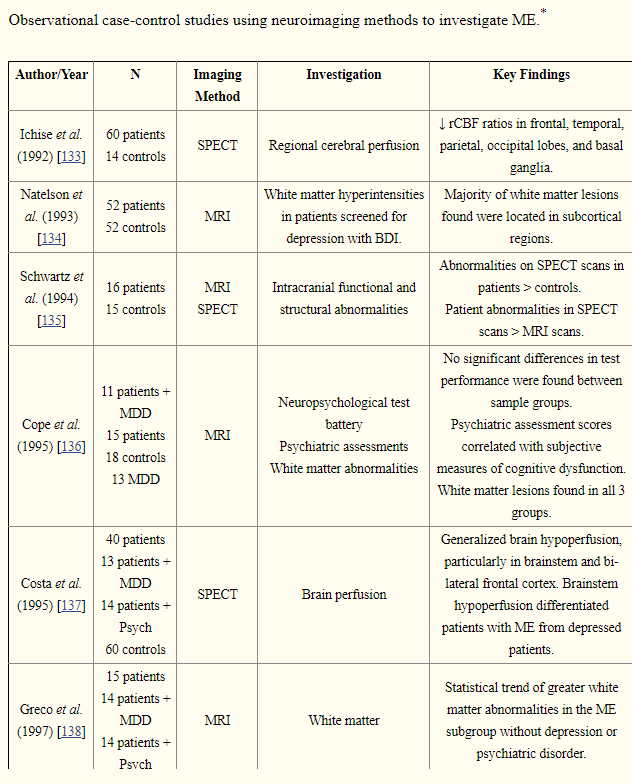
- Brain Scans: See this post for citations from PubMed
- Magnetic resonance imaging (MRI)
- Abnormalities seen in 78% of EBV-associated CFS patients
- Positron Emission Tomography (PET):
- 50% of CFS patients show abnormal scans
- Single-photon emission computerized tomography (SPECT)
- 80% of CFS patients show abnormal scans
- Magnetic resonance imaging (MRI)
- Hypercoagulation [2001]
- 80% of patients had a hypercoaguable state
- 83% of patients had a hereditary abnormality.
- Microbiome (gut bacteria shifts)
- “individuals were classified correctly as ME/CFS with a cross-validation accuracy of 82.93 %.” [See post for citations]
- Review from 2012 (PubMed)
-
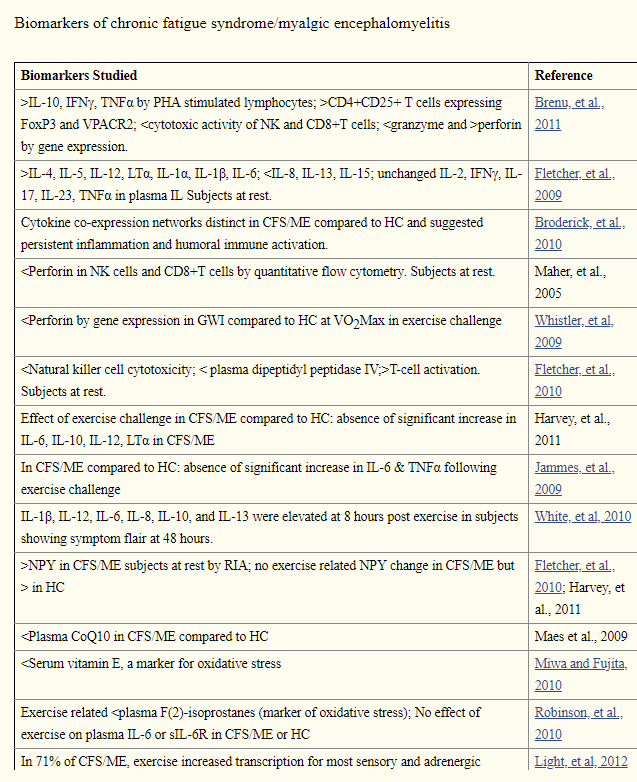
- Review from 2015
-
-
There are multiple markers. If a suspected CFS patient is tested for 2 (hereditary coagulation abnormality and SPECT scan), the odds of both being negative appears to be 3%.
Treatment is a different question — my focus has been on microbiome shifts. Several readers have reported major improvement with this approach — some returning to work (with some symptoms remaining). Fecal Matter Transplants have repeatedly resulted in short term remission — rarely lasted more than 6 months with several readers who have shared their experiences.
Microbiome shifts cannot be resolved with eating yogurt, kefir or even 99% of health food stores probiotics. There are overgrowths that need to reduced and undergrowths that need to be encouraged. At present, uBiome or thryve microbiome tests appear to be the best path forward — with end product production of the microbiome population appearing to be very significant for symptoms seen.
