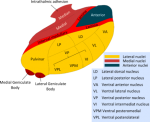
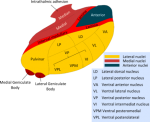
The thalamus has different nuclei, which are only very little connected one to each other. They project to the cortex, and every region in the cortex is projected at from the thalamus. The different nuclei are projected at from regions in the body, and these regions project also to the cortex. These nuclei are the specific nuclei of the thalamus, and participate each exclusively in specific tasks (vision, or whatever). They also get feedback from the cortex.
Yes, I think you're describing how the thalamus serves as a "relay station" that connects all sensory information from the body to the cortical brain. (with the sole exception of the sense of smell) Each type of sensory information is relayed through its own "nucleus" in the thalamus:
But the thalamus is more than just a relay station that provides all the body's sensory information to the cortical brain. As you mention, the cortical brain provides "feedback" nerves to the thalamus, allowing the thalamus to suppress certain sensory information. It is thought that this cortical "feedback" is how the conscious brain decides which sensory information to pay attention to, and which sensory information to ignore. If there is a problem with this "feedback", then the conscious brain may be inundated with too much sensory information. (photophobia, hyperacusis?)
There is another important aspect to the connections between the thalamus and the cortical brain- the aspect of alert consciousness. There is recurring stimulation from the thalamus to the cortical brain and then back to the thalamus, forming a loop. This recurring stimulation through the loop leads to "thalamo-cortical oscillations". Some of these oscillations can be roughly recorded using an electroencephalogram (EEG) as "alpha frequency waves". These alpha frequency waves in EEG typically represent a state of alert consciousness. If there is a problem with the thalamo-cortical oscillations, it may be hard to maintain a state of alert consciousness. (brain fog?)
EEG studies in ME have had a hard time documenting specific abnormalities. But one study noted that "In the eyes closed condition, peak alpha frequency (the frequency between 8 to 13 Hz at which the greatest amount of energy was observed) correlated negatively with the 'fatigue today' rating." This means that patients who reported more fatigue had slower alpha-frequency waves.[1] And a 2014 conference presentation "found decreased [peak alpha frequency] over 58% of the entire cortex in CFS patients when compared to controls. [...] These findings are consistent with reduced efficiency of thalamo-cortical connections in CFS participants." [2]
For those interested, here is one of the earliest papers that established a link between the speed of thalamo-cortical oscillations and attention or information processing:
EEG-alpha rhythms and memory processes (Klimesch, 1997)
The author's later work expands on how thalamo-cortical oscillations are involved in both attention/concentration and in information processing/retrieval:
So, I think this is CFS, and maybe some other badly understood diseases like depression or functional neurological disorders, or whatever. And this (re-) production of healthy or non-healthy shapes of synaptical connections cannot already be shown, nor by PET, nor by MRT, probably as well not by post mortem investigations. Or would it be possible by any of these techniques?
It sounds like you are suggesting that there may be some "re-wiring" of the neuronal connections in ME. You are right that we can't easily detect such "re-wiring" of neuronal connections using PET or MRI. But the function of a neuronal circuit can be changed even without any "re-wiring".
To use an electrical circuit analogy, if one of the wires in the circuit experiences a large increase in resistance, the output of the circuit will change, even without any re-wiring. If the frequency of the circuit's clock/oscillator changes, then the output of the circuit will change, even without any re-wiring.
So a hope could be to find any abnormality in the distribution of Zn, Al, Cr, Ni and Mn (my impression, with at least some possible reasoning); as well as of Vit B2, B1, B7, B5, B3 and B6.
Yes, it would certainly be interesting to examine the abnormalities in the level or distribution of essential nutrients. Both neuroinflammation as well as classical inflammation trigger changes in the levels of nutrients in the area of inflammation, and sometimes in the whole body.
These metabolic changes in neuroinflammation can be different from the metabolic changes seen in classical inflammation. Furthermore, the metabolic changes seen in acute neuroinflammation may be different from the metabolic changes seen in chronic neuroinflammation. But it is indeed important to consider the "downstream" metabolic effects of neuroinflammation.
References
[1]
https://www.tandfonline.com/doi/abs/10.1300/J184v02n02_04
[2]
https://forums.phoenixrising.me/thr...udy-presented-at-stanford.32919/#post-2355997