I thought people might be interested in this piece by Peter White (and a colleague, Anthony Clare - who is dead now) in a medical text book that is very widely used in the UK, and has been translated into other languages.
The index entry for ME directs the reader to the entry for CFS. There is a very small entry in the infectious diseases seciton under the heading Postviral/Chronic Fatigue Syndrome, which states "Studies have suggested that two-thirds of patients with a symptom duration of more than 6 months have an underlying psychiatric disorder".
As CFS wouid normally not be diagnosed within this timeframe, that means basically most of us have a psychiatric reason for our symptoms (according to them).
This section (and the index entry on CFS) then directs then reader to the CFS piece in Section 22 (Psychological Medicine), where CFS/ME is listed nder "Functional or Psychsomatic Disorders: Medically Unexplained Symptoms".
Anyway this is the text below and the details of the book.
Kumar and Clark - Clinical Medicine
By Parveen Kumar, CBE, BSc, MD, FRCP, FRCP (Edin), Professor of
Clinical Medical Education, Barts and The London, Queen Mary's School
of Medicine and Dentistry, University of London, and Honorary
Consultant Physician and Gastroenterologist, Barts and The London NHS
Trust, London, UK; and Michael Clark, MD, FRCP, Honorary Senior
Lecturer, Barts and The London, Queen Mary's School of Medicine and
Denistry, University of London, UK
ISBN 0702027634 Paperback 1528 Pages 1283 Illustrations
Saunders Published August 2005
----------------
Contributors include:
----------------
Anthony W Clare MD FRCPI FRCP FRCPsych MPhil
Professor of Clinical Psychiatry
Trinity College, Dublin;
Medical Director
St Patrick's Hospital, Dublin, Ireland
---------------------------------
Peter D White MD FRCP FRCPsych
Senior Lecturer in Psychological Medicine, Honorary Consultant in
Liaison Psychiatry
Barts and The London, Queen Mary's School of Medicine and Dentistry,
University of London, UK
-----------------------------------
<>
We all have illness behaviour when we choose what to do about a
symptom. Going to see a doctor is generally more likely with more
severe and more numerous symptoms and greater distress. It is also
more likely in introspective individuals who focus on their health.
Abnormal illness behaviour occurs when there is a discrepancy between
the objective somatic pathology present and the patient's response to
it, in spite of adequate medical investigation arid explanation.
FUNCTIONAL OR PSYCHOSOMATIC DISORDERS: MEDICALLY UNEXPLAINED SYMPTOMS
`Functional' disorders are illnesses in which there is no obvious
pathology or anatomical change in an organ (thus in contrast
to `organic and there is a presumed dysfunction in an organ or
system. The word psycho-somatic has had several meanings, including
psychogenic, `all in the mind'; imaginary and malingering. The modern
meaning is that psychosomatic disorders are syndromes of unknown
aetiology in which both physical and psychological factors are likely
to be causative, The psychiatric classification of these disorders
would be somatoform disorders, but they do not fit easily within
either medical or psychiatric classification systems, since they
occupy the hinterland between them. Medically unexplained symptoms
and syndromes are very common in both primary care and the general
hospital (over half the outpatients in gastroenterology and neurology
clinics have these syndromes). Because orthodox medicine has not been
particularly effective in treating or understanding these disorders,
many patients perceive their doctors as unsympathetic and seek out
complementary treatments of uncertain efficacy. Examples of
functional disorders are shown in Table 22.4.
Because epidemiological studies suggest that having one of these
syndromes significantly increases the risk of having another, some
doctors believe that these syndromes represent different
manifestations in time of `one functional syndrome', which is
indicative of a somatization process. Functional disorders also have
a significant association with psychiatric disorders, especially
depressive and panic disorders as well as phobias. Against this view
is the evidence that the majority of primary care patients with most
of these disorders do not have either a psychiatric disorder or other
functional disorders.
Table 224
Functional or psychosomatic syndromes (medically unexplained symptoms)
`Tension' headaches
Atypical facial pain
Atypical chest pain
Fibromyalgia (chronic
widespread pain)
Other chronic pain syndromes
Chronic or post-viral fatigue syndrome
Multiple chemical sensitMty
Premenstrual syndrome
Irritable or functional bowel syndrome
Irritable bladder syndrome
It also seems that it requires a major stress or a psychiatric
disorder in order for such sufferers to attend their doctor for help,
which might explain why doctors are so impressed with the
associations with stress and psychiatric disorders. Doctors have
historically tended to diagnose `stress' or `psychosomatic disorders'
in patients with symptoms that they cannot explain. History is full
of such disorders being reclassified as research clarifies the
pathology. A recent example is writer's cramp (p. 1233) which most
neurologists now agree is a dystonia rather than a neurosis.
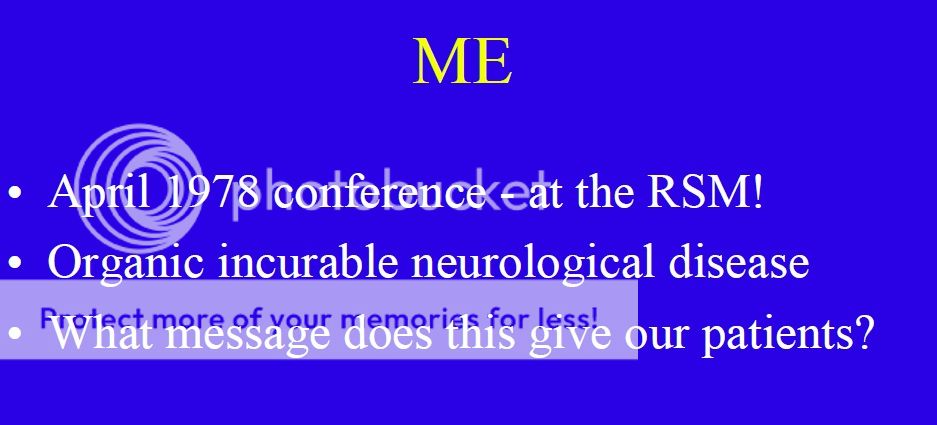
Chronic fatigue syndrome (CFS)
There has probably been more controversy over the existence and
aetiology of CFS than any other functional syndrome in recent years.
This is reflected in its uncertain classification as neurasthenia in
the psychiatric classification and myalgic encephalomyelitis (ME)
under neurological disorders. There is good evidence for this
syndrome, although the diagnosis is made clinically and by exclusion
of other fatiguing disorders. Its prevalence is 0.5% in the UK,
although abnormal fatigue as a symptom occurs in 10-20%. It occurs
most commonly in women between the ages of 20 and 50 years old, The
cardinal symptom is chronic fatigue made worse by minimal exertion.
The fatigue is usually both physical and mental, with associated poor
concentration, impaired registration of memory, irritability,
alteration in sleep pattern (either insomnia or hypersomnia), and
muscular pain. The name myalgic encephalomyelitis (ME) is
decreasingly used within medicine because it implies a pathology for
which there is no evidence.
Aetiology
Functional disorders often have aetiological factors in common with
each other (see Table 22.5), as well as more specific aetiologies.
For instance, CFS can be triggered by certain infections, such as
infectious mononucleosis and viral hepatitis. About 10% of patients
with infectious mononucleosis have CFS 6 months after the infectious
onset, yet there is no evidence of persistent infection in these
patients. Those fatigue states which clearly do follow on a viral
infection can be classified as post-viral fatigue syndromes. Other
aetiological factors include physical inactivity arid sleep
difficulties. immune and endocrine abnormalities noted in CFS may be
secondary to the inactivity or sleep disturbance commonly seen in
patients. Mood disorders are present in a large minority of patients,
and can cause problems in diagnosis because of the large overlap in
symptoms. These mood disorders may be secondary, independent (co-
morbid), or primary with a misdiagnosis of CFS. The role of stress is
uncertain, with some indication that the influence of stress is
mediated through consequent psychiatric disorders exacerbating
fatigue, rather than any direct effect.
Management
The general principles of the management of functional disorders are
given in Box 22.7. Specific management of CFS should include a
mutually agreed and supervised programme of gradual increasing
activity However, few patients regard themselves as cured after
treatment. It is sometimes difficult to persuade a patient to accept
what are inappropriately perceived as psychological therapies' for
such a physically manifested condition. Antidepressants do not work
in the absence of a mood disorder or insomnia.
Prognosis
This is poor without treatment, with less than 10% ot hospital
attenders recovered after 1 year Outcome is worse with increasing
age. co-morbid mood disorder, and the conviction that the illness is
entirely physical.
Table 22.5 Aetiological factors commonly seen in functional disorders
Predisposing
Perfectionist obsessional and introspective personality
Childhood traumas (physical and sexual abuse)
Similar illnesses in first-degree relatives
Precipitating (triggering)
Infections
Chronic fatigue syndrome (CFS)
irritable bowel syndrome (IBS)
Psychologically traumatic events (especially accidents)
Physical Injuries ('fibromyalgia and other chronic pain syndromes)
Life events that precipitate changed behaviours (e.g. going off sick)
Incidents where the patient believes others are responsible
Perpetuating ( maintaining)
Inactivity with consequent physiological adaptation (CFS
and 'fibromyalgia').
Avoidant behaviours multiple chemical sensitivities (MCS) CFS
Maladaptive illness beliefs (that maintain maladaptive behaviours)
(CFS)
Excessive dietary restrictions (`food allergies')
Stimulant drugs
Sleep disturbance
Mood disorders.
Somatization disorder
Unresolved anger or guilt
Unresolved compensation
Box 22.7 Management of functional disorders
The first principles is the identification and treatment of
maintaining factors (e.g. dysfunctional beliefs and behaviours mood
and sleep disorders)
Communication
Explanation of ill-health, including diagnosis and causes
Education about management (including self-help leaflets) .
Stopping drugs (e. g. caffeine causing insomnia, analgesics causing
dependence)
Rehabilitative therapies
Cognitive behaviour therapy (to challenge unhelpful beliefs and
change coping strategies)
Supervised and graded exercise therapy for approximately 3 months (to
reduce inactivity and improve fitness)
Pharmacotherapies
Specific antidepressants for mood disorders,analgesia and sleep
disturbance .
Symptomatic medicines (e.g. appropriate analgesia, taken only when
necessary)
-------------------------------------------------