Hi everyone,
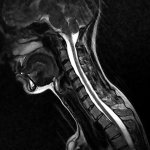
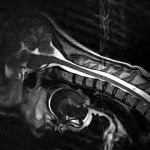
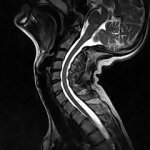
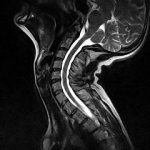
My sister received her report from Dr Gilete - CCI , AAI and subaxial instability C4-C5. He recommended surgery.
Before taking any decision I really feel that I have to have another opinion. We are from Europe. Any advice to contact the other doctors Bolognese and Henderson ? Is there a long waiting list? How long it would take to have an answer from them? Any of them agrees with video conferences because is impossible for us to travel to USA?
Thank you. I am grateful for any info.
My sister received her report from Dr Gilete - CCI , AAI and subaxial instability C4-C5. He recommended surgery.
Before taking any decision I really feel that I have to have another opinion. We are from Europe. Any advice to contact the other doctors Bolognese and Henderson ? Is there a long waiting list? How long it would take to have an answer from them? Any of them agrees with video conferences because is impossible for us to travel to USA?
Thank you. I am grateful for any info.
Last edited: