my whole „theory“ stands on the idea that people will have greater results post surgery if there is brainstem compression which seems somewhat more likely in more pronounced vertical instability, this seems to be a different kind of injury to the nerve tissue than a stretch injury, which seems more likely (or solely happening?) in horizontal instability.
If you look at classic spinal cord accidents it is mostly a stretch injury (or tear in worst case) which results in mostly irreversible (?) damage- also due to the massive inflammatory cascade which ensues thereafter. So maybe that is similar?
Ok, now I think, I got you. And indeed, its reasonable to me, that stretching could be much more likely irreversible than compressing. If I recognize rightly,
@JenB was diagnosed by dynamic BDI and thereby with vertical instability. So, that would make sense. But I remember
@jeff_w mentioned, that he had a retroflexed odontoid, what would be considered as horizontal instability, as far as in understand.
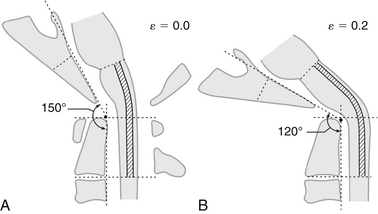
What I'm wondering about as well is the following. Grabb Oakes seems more sensitive to horizontal instability. (
https://me-pedia.org/wiki/Craniocervical_instability#Measurements ) And that makes a lot of sense. Grabb Oakes is for example pathological, if odontoid dip into brainstem/ spinal cord (sorry, no idea where the one ends exactly and the other begins). That would make CXA pathological in many cases, as well. But, what I'm trying to say, considering Henderson, Grabb Oakes implies brainstem compression. (
https://www.omicsonline.org/open-ac...ty-connective-disorders-2165-7939-1000299.pdf page 2) So, in that case a horizontal instability would lead to brainstem compression, if I gout everythin right.
Everybody has to understand that I am a baker, not a doctor or scientist, I constructed this „theory“ from a very limited data set and years of reading personal anectodal accounts of patients. I basically have no idea what I am talking about and looking back reading posts here while getting sicker and sicker with trying things I wish that I have known that nobody else does either.
Matties description of his improvement fits the available data more than the „miracle“ patients, I have zero doubt that they are real but we have to understand why they got so much better before assuming that everyone (or even the biggest part of patients) will have these incredible results!
I've got a Ph. D.* and I'm not any smarter than you. It doesn't matter what you are. (Anyway, baker is a great profession, In my opinion.) We're all here for the same reason, helping each other. And your critical way of thinking is very helpful. I think, everyone here appreciate this.
* In engineering, what most people would not consider as science.