interesting - thanks Hip
i am having trouble getting clarity on how far into the structure the mucous membrane reaches
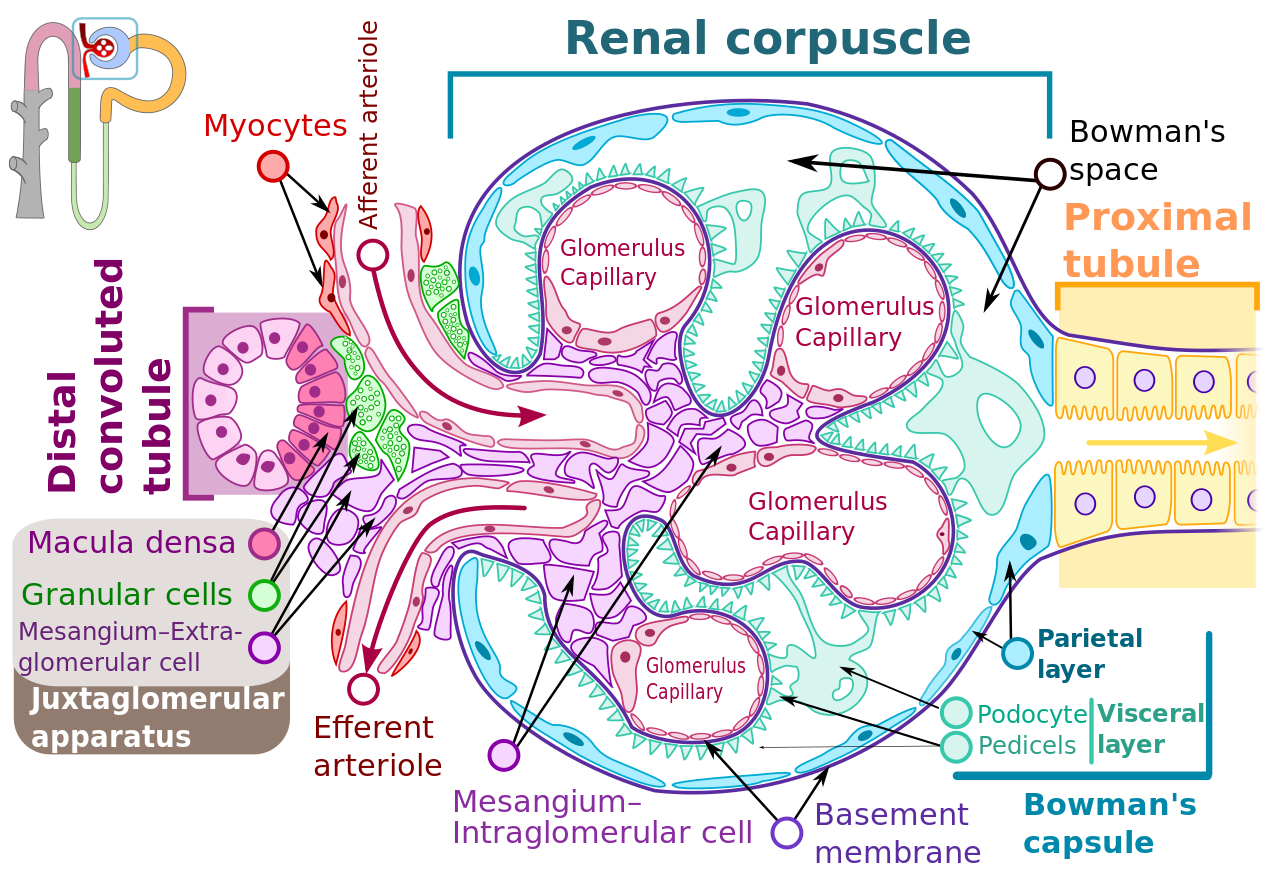
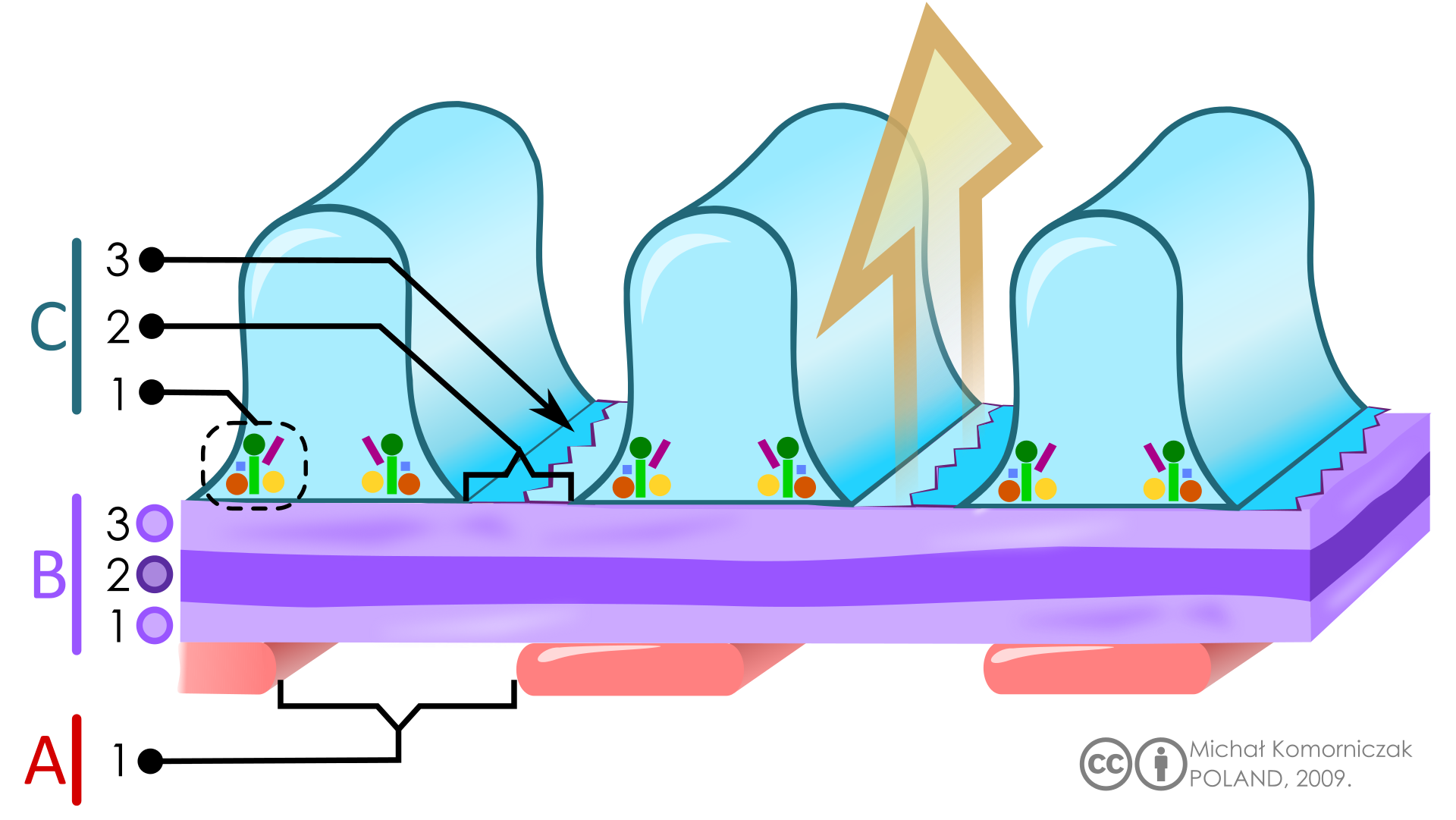
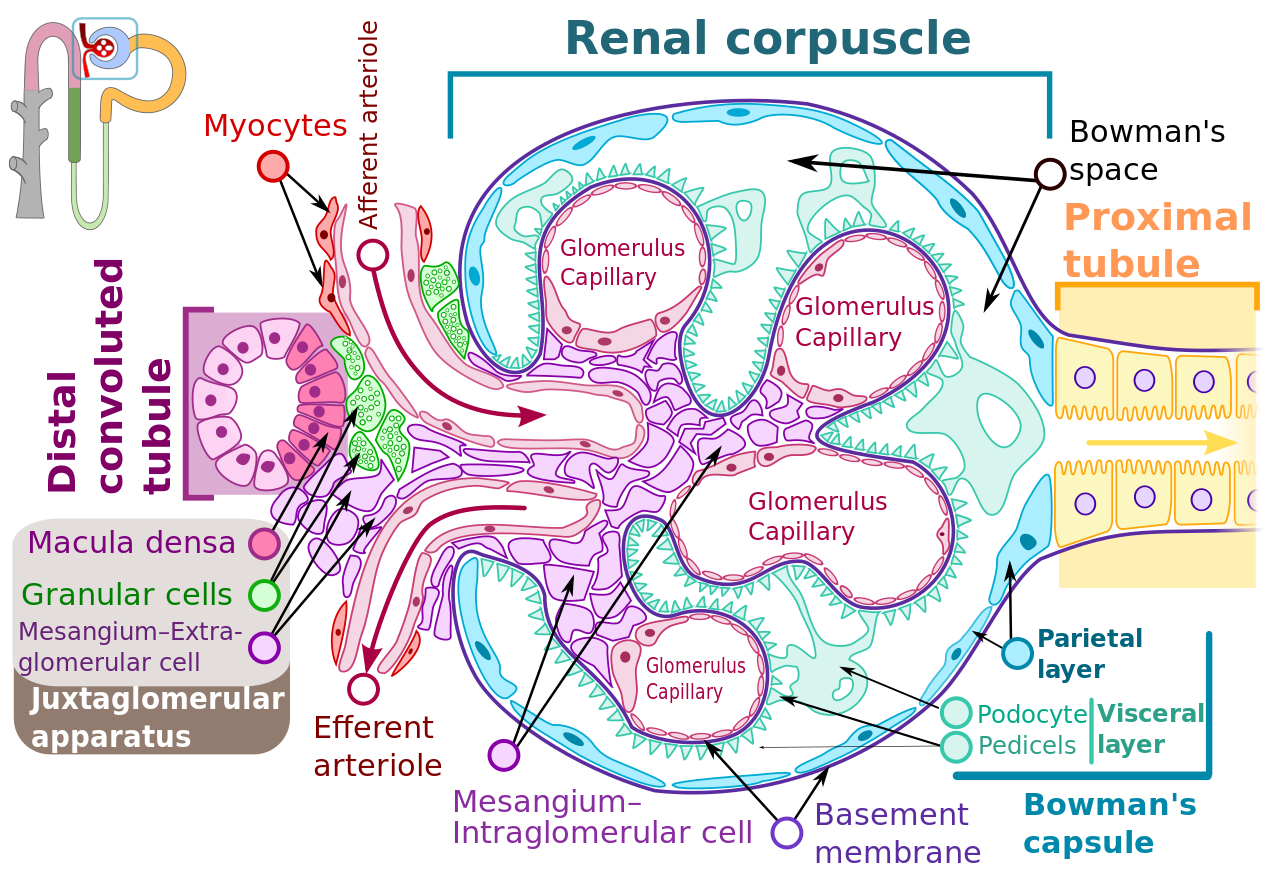
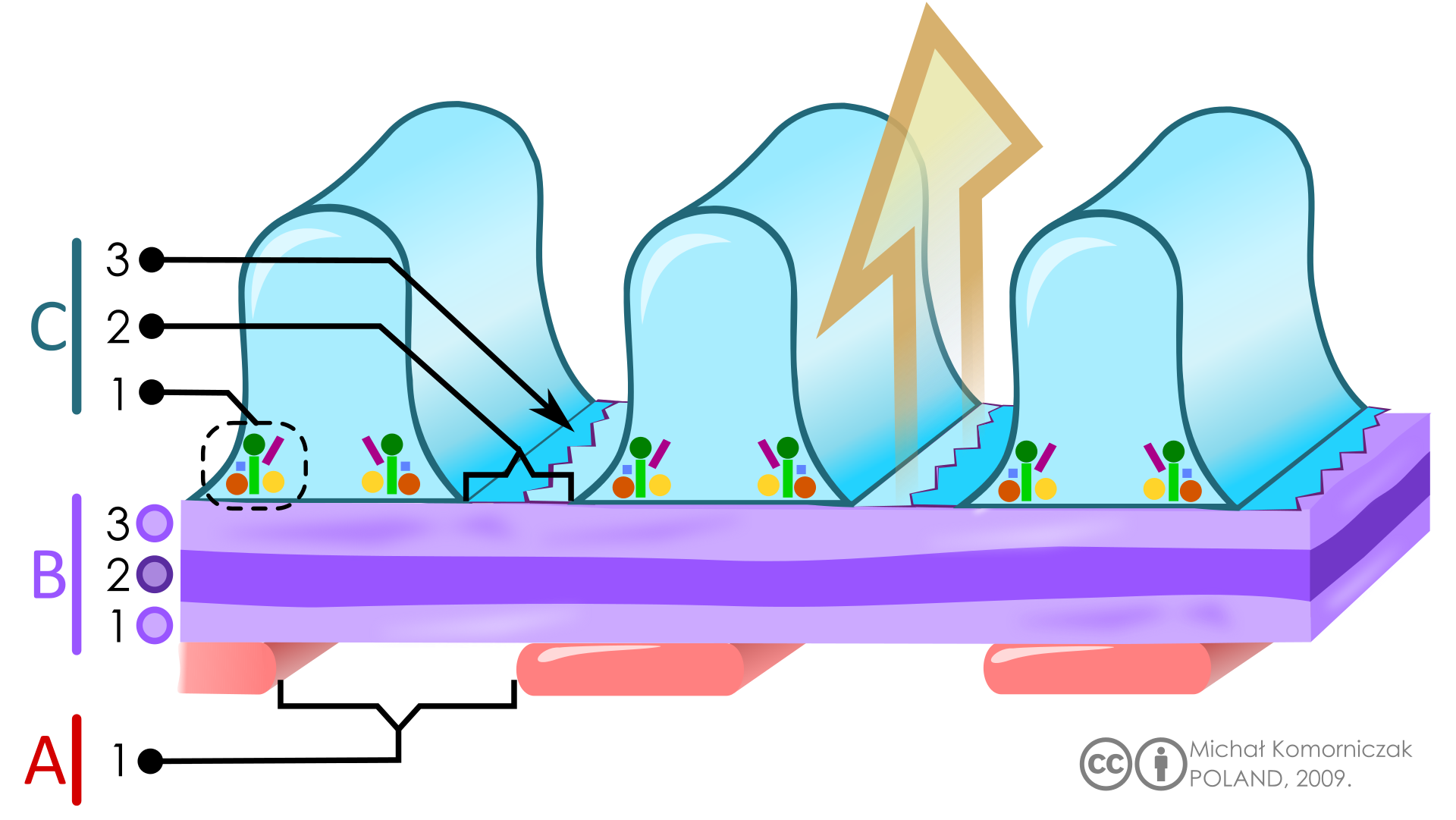
here is a diagrammatic representation of the filtration membrane inside the bowman's capsule - it doesn't look to me like there is a mucosa there as such - just the specialised filtration membrane at the boundary between the blood flow and the urine side
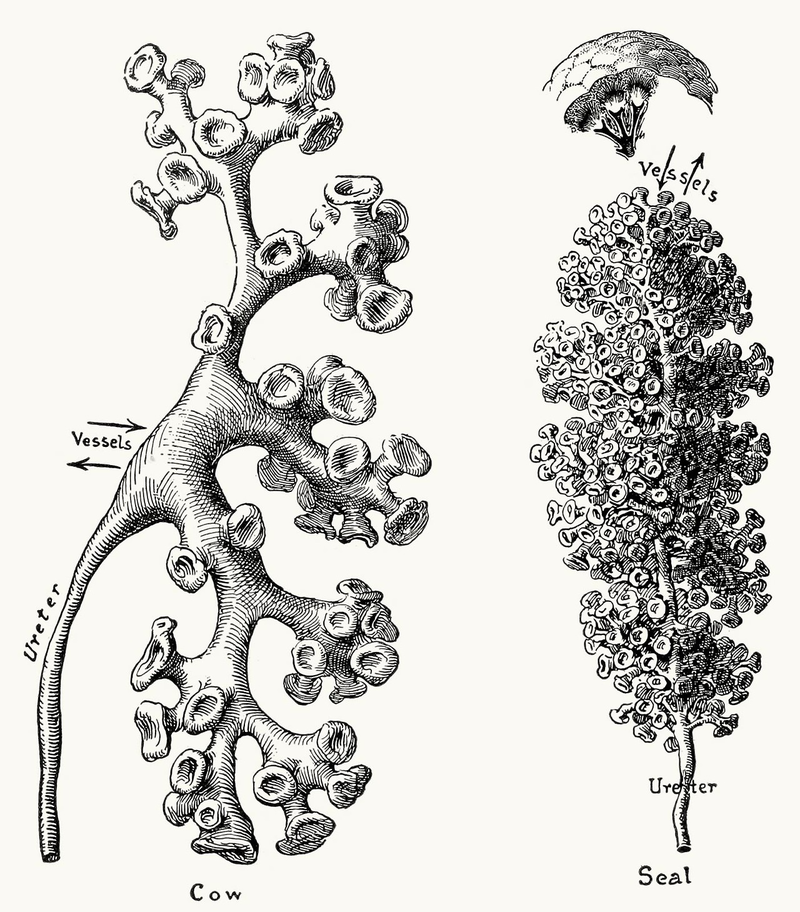
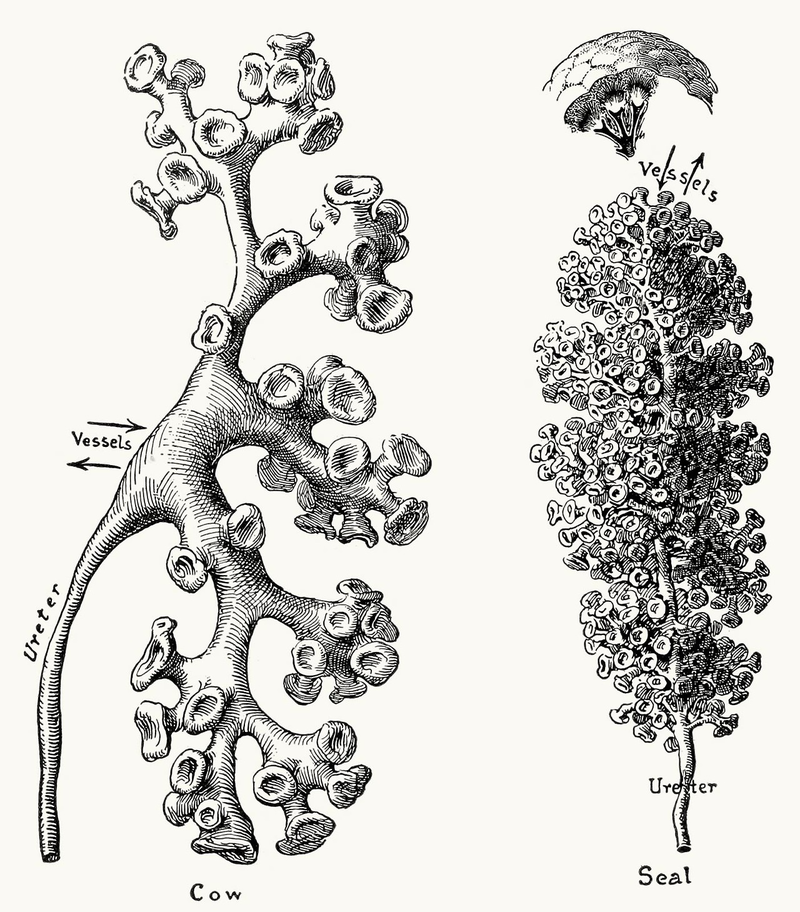
its clear that the ureters and bladder all have true mucous membranes - so zooming out to the broader structure of the kidney and working in from the urine side - the ureters branch into the the renal calyces which are chambers of the kidney through which urine collects from the passes.
these are little cup shaped voids that collect and i think pump the urine out down the ureters to the bladder. they are of interest to us here as they are the usual site of standard kidney infections so these are perhaps the prime candidates for the location of Markov's proposed biofilm infection
its not clear to me yet how much further into the structure of the kidney the mucosa might reach - this image shows the proximal tubule where the urine comes out of the bowman's capsule - that may also have a mucosal membrane - but there doesn't seem to be any physical barrier between that space and the insde of the bowmans space - so any bacterial there could presumably make it inside the bownam's space also
i am having trouble getting clarity on how far into the structure the mucous membrane reaches
here is a diagrammatic representation of the filtration membrane inside the bowman's capsule - it doesn't look to me like there is a mucosa there as such - just the specialised filtration membrane at the boundary between the blood flow and the urine side
its clear that the ureters and bladder all have true mucous membranes - so zooming out to the broader structure of the kidney and working in from the urine side - the ureters branch into the the renal calyces which are chambers of the kidney through which urine collects from the passes.
these are little cup shaped voids that collect and i think pump the urine out down the ureters to the bladder. they are of interest to us here as they are the usual site of standard kidney infections so these are perhaps the prime candidates for the location of Markov's proposed biofilm infection
its not clear to me yet how much further into the structure of the kidney the mucosa might reach - this image shows the proximal tubule where the urine comes out of the bowman's capsule - that may also have a mucosal membrane - but there doesn't seem to be any physical barrier between that space and the insde of the bowmans space - so any bacterial there could presumably make it inside the bownam's space also