You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Pyruvate dehydrogenase function depends on thiamine (B1)
- Thread starter Chocolove
- Start date
I have a dilemma : I am chelating lead but it also pulls magnesium which is already low.....w/out magnesium I cannot restore B1
What to do?
I don't have advice for you on what to do. However, there does appear to be some relationship between lead (Pb) and B1.
Influences of thiamin on lead intoxication, lead deposition in tissues and lead hematological responses of Tilapia zillii
Treatment of lead toxicity in calves
Nutrition to Fight Lead Poisoning
The therapeutic potential of thiamine for treatment of experimentally induced subacute lead poisoning in sheep
Effect of Ascorbic Acid and Thiamine Supplementation at Different Concentrations on Lead Toxicity in Liver
Interestingly, I had an unprovoked and provoked metals test. Lead (Pb) was the only metal slightly elevated. I am also B1 deficient. Interesting coincidence?
Last edited:
Chocolove
Tournament of the Phoenix - Rise Again
- Messages
- 548
We aren't knowledgeable of all your circumstances and a good nutritionist might be of considerable help rebuilding your magnesium stores.I have a dilemma : I am chelating lead but it also pulls magnesium which is already low.....w/out magnesium I cannot restore B1
I would think that examination of your diet/drink/medication may help expose why you are low in magnesium and how to increase absorption. Currently, an estimated 75% of Americans have daily magnesium intakes less than the RDA4 , with similar figures estimated for most industrialized nations. But beyond the generalization that Americans have low magnesium intake to begin with there are substantial and common dietary issues that block magnesium absorption through the gut, such as:
More details and references are available in this article see: http://www.ancient-minerals.com/magnesium-sources/absorption/One example of a diet high in minerals found to impair magnesium bioavailability would be one high in both milk and phosphorous-containing carbonated beverages, such as colas. For those with a regular daily intake of carbonated beverages, it may be wise to find additional sources of magnesium to supplement intake and prevent deficiency...
In one study, addition of 300 to 1000 mg of calcium to the diet decreased magnesium absorption significantly in participants consuming an average of 370 of dietary magnesium daily.6
Minerals are generally known to have an antagonistic or competitive effect when it comes to absorption. Thus high intake of any of the following minerals could potentially reduce magnesium bioavailability:
- Calcium
- Phosphorous
- Iron
- Copper
- Manganese
Foods that hinder magnesium absorption include:
The above list should be viewed with caution and reservation when selecting foods, however. In many cases, foods that contain high fiber, phytic acid or oxalic acid are also high in absorbable forms of magnesium.
- Non-fermentable or insoluble fiber, such as whole grain, bran and seeds
- Foods high in phytates, such as whole flours and grains, bran, the hulls of seeds and nuts, and un-sprouted beans and soy
- Foods high in oxalates, such as spinach, leafy greens, nuts, tea, coffee and cacao
For example, choosing high fiber grains, which are high in magnesium, will typically provide better intake and absorption of magnesium than choosing low fiber grains that are low in magnesium, including processed breads made from white flour.
Certain cooking methods can lessen the negative impact of phytates and oxalates on absorbable magnesium. For example, traditional diets commonly include sprouted and fermented grains and legumes. Scientists have now recognized the ability of these techniques to reduce the ability of phytic acid to bond with magnesium.
Cooking reduces oxalic acid, and in one study a diet of cooked spinach was found to have higher absorption than a diet of raw spinach.6 Though cooking also reduces water-soluble vitamins, water-soluble vitamins also tend to be plentiful in foods that are not high in magnesium.
The following cooking procedures, therefore, can increase magnesium absorption:
In addition, it generally follows that foods with diuretic properties, such as coffee, tea and alcohol, tend to reduce available magnesium in the bloodstream, due to the action of these foods to increase the excretion of fluids by the kidneys.6 9 10
- Soaking grains and beans before cooking
- Sprouting beans
- Cooking foods high in oxalic acid, such as spinach and leafy greens, rather than eating them raw
Low magnesium in the body is a very serious situation since the body depends on it in so many ways. I think you are very wise to check into this.
Asklipia
Senior Member
- Messages
- 999
Thank you @Chocolove for taking the trouble to write this excellent post! 
Found this interesting nugget (source link):
I'm functionally deficient in B3 and I was borderline deficient in B9 per SpectraCell testing.
Folate deficiency
Thiamine serves as a coenzyme (in the form of thiamine pyrophosphate) in a variety of metabolic processes. In these processes, thiamine pyrophosphate is regenerated via the donation of a proton from the reduced form of nicotinamide adenine dinucleotide (NADH).
Folic acid is essential to having enough dihydrofolate reductase to regenerate NADH from its oxidative form. This regeneration allows NADH to continue to be present to regenerate thiamine pyrophosphate without being consumed in the process.
If folic acid is deficient in cells, it causes an indirect thiamine deficiency, because thiamine is present but cannot be activated.
I'm functionally deficient in B3 and I was borderline deficient in B9 per SpectraCell testing.
Last edited:
I'm functionally deficient in B3 and I was borderline deficient in B9 per SpectraCell testing.
Not sure if Spectracell testing is very accurate: I had it done in 2012 and my vitamin C levels came back well within the 'normal' range, despite clear physical signs of outright scurvy. My glutathione was high-normal, but it didn't distinguish between oxidized or reduced, and my 'Immunidex' score was 85 out of 100, indicating (according to them) that I have a 'very strong cell-mediated immune response'.
Note that it's the one part of the article which is completely uncited. They have provided no basis for that claim.Found this interesting nugget (source link):
Hello All,
Some thoughts for discussion and would love to hear other's thoughts...

Cholinergic Deficiency Hypothesis in Delirium: A Synthesis of Current Evidence - Link
Some thoughts for discussion and would love to hear other's thoughts...
- B1 is required for pyruvate dehydrogenase (PDH) enzyme. [Source]
- PDH is also involved in the production of acetylcholine, a neurotransmitter, and for myelin synthesis. [Source]
- Anticholinergics block the neurotransmitter acetylcholine in the central and the peripheral nervous system. [Source]
- The list of drugs that have Anticholinergic properties is long.
- Could some of the common OTC and prescription medications that are anticholinergic be affecting those that are B1 deficient? If so, how?
- Has anyone heard of or completed a serum anticholinergic activity (SAA) test?

Cholinergic Deficiency Hypothesis in Delirium: A Synthesis of Current Evidence - Link
Acetylcholine is produced from the interaction of choline with acetyl coenzyme A (CoA). Thus, dysfunctions in this pathway or reductions in precursor availability can diminish acetylcholine levels (11,15). Acetyl CoA is produced by glucose breakdown in the citric acid cycle. Consequently, hypoglycemia or severe malnutrition may also lead to cholinergic deficit. In experimental animals, vulnerable steps include glucose breakdown, NAD+ and NADP generation from niacin, and enzyme synthesis from thiamine (Figure 2, Item 2) (16). Moreover, thiamine deficiency prevents turnover, leading to selective apoptosis of cholinergic neurons in animal models (Figure 2, Item 3) (17).
Last edited:
Chocolove
Tournament of the Phoenix - Rise Again
- Messages
- 548
@JasonUT
When we put drugs into the body instead of repleting nutritional deficiencies there are so many consequences... deciphering symptom cause becomes exponentially harder.
Back to thiamine deficiency.
Certain things like alcohol and diuretic drug deplete thiamine. Here is a sample chart of what happens from the resulting thiamine deficiency:
The Chart Below Illustrates Common Consequences of Thiamine Deficiency:
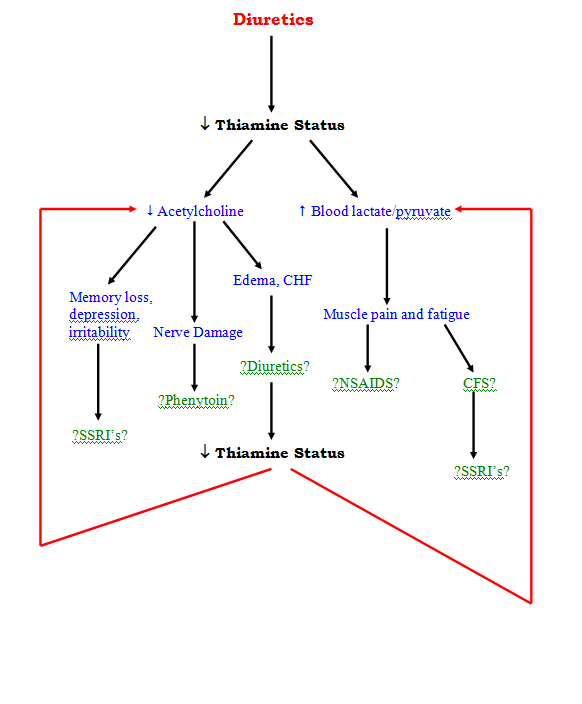
**Key
SSRI’s = Selective serotonin reuptake inhibitors (meds used to treat depression – prozac, paxil, zoloft, etc)
NSAIDS – Non steroidal inflammatory drugs (aspirin, ibuprofen, etc)
CFS – Chronic fatigue syndrome
CHF – Congestive heart failure
From: http://towncenterwellness.com/learning-center/vitamins-and-mineral-info/vitamin-b1-thiamin/
**********************************************************************************************************************
So perhaps from depression caused by a nutrient deficiency one ends up going to a doctor who prescribes anti-depressant drugs like SSRIs rather than first treating with nutrients/vitamins. Now what are the consequences from taking the SSRI? Generally speaking...
Check out this article: http://thenatpath.com/mind/depression/taking-antidepressants-the-top-3-must-have-nutrients/
by Dr. Nicole Cain, ND, MA Posted May 7, 2015
But of course the above article is a generalization...it may or may not apply to sertraline...ZOLOFT® (sertraline hydrochloride)
Here is one anecdotal incident that may or may not be relevant:
"A Case of a Vision Disorder
As of 2011, there are no group studies of the interaction of the SSRI Zoloft and melatonin, but a case study published in the December 1999 issue of “Journal of Neuro-Ophthalmology” suggests that Zoloft together with melatonin and a high-protein diet can be a risky cocktail. The patient had taken Zoloft for four years but had started a high-protein diet and a melatonin supplement two weeks before her examination. At the time of the examination, she experienced loss of clarity of vision, color disturbances and altered light adaptation.
When the high-protein diet and the melatonin supplement were discontinued, her vision improved. Given the possible interactions between Zoloft and melatonin, the researchers recommend against mixing the two, particularly while eating a high-protein diet."
as mentioned in http://www.livestrong.com/article/444220-is-it-safe-to-take-melatonin-with-ssris/
***************
You may want to check out the adverse events reported in the year 2016-2017 while taking sertraline as shown in a pie chart here:
https://www.recallguide.org/drug/zoloft/
It certainly does get complicated.
I am taking two drugs with anticholinergic properties, sertraline
- How could some of the common OTC and prescription medications that are anticholinergic be affecting those that are B1 deficient?
I’m not sure why more psychiatrists don’t first test for nutritional deficiencies before dispensing Zoloft or Prozac,...
10 Nutritional Deficiencies That May Cause Depression
http://www.everydayhealth.com/colum...ional-deficiencies-that-may-cause-depression/
When we put drugs into the body instead of repleting nutritional deficiencies there are so many consequences... deciphering symptom cause becomes exponentially harder.
Back to thiamine deficiency.
Certain things like alcohol and diuretic drug deplete thiamine. Here is a sample chart of what happens from the resulting thiamine deficiency:
The Chart Below Illustrates Common Consequences of Thiamine Deficiency:
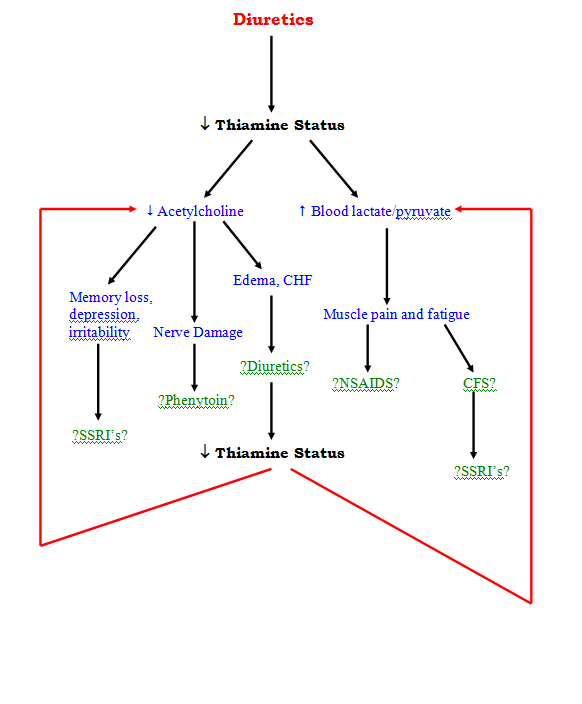
**Key
SSRI’s = Selective serotonin reuptake inhibitors (meds used to treat depression – prozac, paxil, zoloft, etc)
NSAIDS – Non steroidal inflammatory drugs (aspirin, ibuprofen, etc)
CFS – Chronic fatigue syndrome
CHF – Congestive heart failure
From: http://towncenterwellness.com/learning-center/vitamins-and-mineral-info/vitamin-b1-thiamin/
**********************************************************************************************************************
So perhaps from depression caused by a nutrient deficiency one ends up going to a doctor who prescribes anti-depressant drugs like SSRIs rather than first treating with nutrients/vitamins. Now what are the consequences from taking the SSRI? Generally speaking...
Check out this article: http://thenatpath.com/mind/depression/taking-antidepressants-the-top-3-must-have-nutrients/
by Dr. Nicole Cain, ND, MA Posted May 7, 2015
...Antidepressants deplete your body of mood-regulating neurotransmitters.
- Antidepressants deplete your body of nutrients that are essential for brain function and neurotransmitter production.
- Supplementation can help curb side effects of antidepressant medications
- Top 3 nutrients you should add to your regimen: Melatonin, Coenzyme Q10, and B Vitamins.
Common scenario with antidepressant medications
Patients all too often experience the following scenario: Richard goes to his doctor with moderate depression. He is started on fluoxetine (Prozac) by his primary care physician. Within two weeks Richard’s mood starts to improve, however six to nine months later his symptoms start to slip and he is feeling worse again. He goes back to his physician and they increase the dosage of his medication. While this works for a little while, eventually Richard’s depression returns—this time, however, it is worse than it had been in the beginning. He goes back to his physician desiring to discontinue the medication because it is making him severely depressed, he also now has insomnia and anxiety. However, weaning off makes his symptoms even worse.
The antidepressant that Richard was taking is a selective serotonin re-uptake inhibitor (SSRI). SSRI’s do not aid in the brain making serotonin, but rather they prevent the body from deactivating serotonin, which increases the number of neurotransmitters in the brain. This increase stimulates the Monoamine Oxidase (MAO) system in the brain which causes a rapid breakdown of neurotransmitters to compensate with the neurotransmitter overload. In order to build his neurotransmitter stores back up, Richard will need increased amounts of nutrients for neurotransmitter production. Additionally, research shows that fluoxetine also depletes the brain of these nutrients, including melatonin. Richard now has an increased demand for nutrient precursors, and a drug-caused nutrient depletion.1
Gut Psychology
The other way that antidepressant medications impact nutrient levels is through gut psychology or the gut-brain axis. SSRI medications not only affect brain function, but they also impact the digestive tract interfering with your body’s ability to absorb nutrients—in fact research shows that 95 percent of your serotonin receptors are found in your digestive tract. Correspondingly, one of the most common side effects of SSRI medications is digestive upset. A gut that is upset, inflamed, and out of balance is not functioning optimally. Therefore it will not absorb nutrients properly.2
Thusly, Richard now has neurotransmitter breakdown and deficiency, nutrient precursor deficiency, and likely also impaired nutrient absorption. As a result of these factors, Richard is likely going to need more and more medication and higher and higher doses—thusly worsening the cycle by causing more neurotransmitter break down and further nutrient depletion.
If you are taking an antidepressant you will have the best results by optimizing your nutrition with a healthy diet, healing the gut, as well as taking supplements that contain nutrients that are particularly important for neurotransmitter production as well as replenish deficiencies that are caused by your medication.
The top three nutrients to consider supplementing with are: Melatonin, Coenzyme Q10 (COQ10), and B vitamins.
Melatonin, COQ10, and B Vitamins are essential nutrients for your brain and body, but they are just the beginning. As discussed, antidepressant medications may be benifical at the onset, but they can cause a cascade of downstream effects that may be detramental to your health....
- Melatonin: Melatonin is an important hormone that is secreted by your pineal gland and is involved with not only your sleep-wake cycle, but it is also important in your hormone balance and reproductive cycle. As mentioned above, antidepressant medications can deplete your body of melatonin.3,4 If your melatonin becomes depleted you my start to suffer from disturbances in your sleep including difficulty falling asleep, and frequent waking. Supplementation with at least 3 mg before bed may help replenish your melatonin stores. It is also a safe, and effective way to help you fall asleep and sleep through the night.
- Coenzyme Q10 (COQ10): COQ10 is found in every cell of your body. It enables the cells to produce energy so that they can grow as well as maintain the body’s functions. COQ10 is also a powerful antioxidant and protects the body and brain from damage. Studies show that tricyclic antidepressants, among others, deplete COQ10 stores.5 This can cause brain fog, mental fatigue, difficulty concentrating, memory lapses, depression, irritability and more.6 Supplementation with at least 100 mg will replenish your COQ10 stores, and it will help your cells have the energy they need for brain and body function.
- B Vitamins: B vitamins are essential for brain function and mood regulation. For example: Vitamin B12 (cobalamin) helps your body make the fatty layer called myelin that surrounds the nerve cells in your brain. This helps your brain send signals which affects your ability to think, concentrate, remember, and it also impacts your mental health. Another example is B6 (pyridoxine), which is involved in sleep, nerve function, carrying oxygen in the red blood cell, and much more.
- Antidepressant medications can deplete your body of your B Vitamins, thusly impacting your brain function and overall health. An example of this are tricyclic antidepressants, which deplete your brain and body of vitamin B2 (riboflavin) which can affect mood, sleep, memory and more. Supplementation with a good B Complex vitamin will help your brain and body reach it’s optimal potential.7
Kaslow, J. MD. (2015) HOW SSRI’S DEPLETE NEUROTRANSMITTER LEVELS. drkaslow.com. Retrieved on 4/1/15 from http://www.drkaslow.com/html/neurotransmitter_depletion.html
Hadhazy, A. (2010, February 12). Think Twice: How the Gut’s “Second Brain” Influences Mood and Well-Being. Retrieved September 13, 2014 from: http://www.scientificamerican.com/article/gut-second-brain/
Drugs that Deplete: Melatonin. (2011). PennState Hershey. MIlton S. Hersehey Medical Center. Retrieved on 4/1/15 from http://pennstatehershey.adam.com/content.aspx?productId=107&pid=33&gid=000712
Drugs that Deplete: Coenzyme Q102011). PennState Hershey. Milton S. Hersehey Medical Center. Retrieved on 4/1/15 from http://pennstatehershey.adam.com/content.aspx?productId=107&pid=33&gid=000706
...
But of course the above article is a generalization...it may or may not apply to sertraline...ZOLOFT® (sertraline hydrochloride)
Here is one anecdotal incident that may or may not be relevant:
"A Case of a Vision Disorder
As of 2011, there are no group studies of the interaction of the SSRI Zoloft and melatonin, but a case study published in the December 1999 issue of “Journal of Neuro-Ophthalmology” suggests that Zoloft together with melatonin and a high-protein diet can be a risky cocktail. The patient had taken Zoloft for four years but had started a high-protein diet and a melatonin supplement two weeks before her examination. At the time of the examination, she experienced loss of clarity of vision, color disturbances and altered light adaptation.
When the high-protein diet and the melatonin supplement were discontinued, her vision improved. Given the possible interactions between Zoloft and melatonin, the researchers recommend against mixing the two, particularly while eating a high-protein diet."
as mentioned in http://www.livestrong.com/article/444220-is-it-safe-to-take-melatonin-with-ssris/
***************
You may want to check out the adverse events reported in the year 2016-2017 while taking sertraline as shown in a pie chart here:
https://www.recallguide.org/drug/zoloft/
It certainly does get complicated.
Dr. Lonsdale's thoughts on anti-cholinergic drugs with relation to B1 deficiency - Link
Derrick Lonsdale says:
August 17, 2017 at 11:41 am
I don’t know anything about the drugs because I never used them. Thiamin deficiency will result in loss of cholinergic neurotransmitter drive. I cannot think of anything less likely to help you by taking an “anti-cholinergic drug” because cholinergic drive is extremely important in many aspects of brain metabolism
Last edited:
Just ordered Londsdale's new book:
Thiamine Deficiency Disease, Dysautonomia, and High Calorie Malnutrition
This article has a 30% discount code. It's still expensive, but I plan to let my docs borrow it after I am finished. Hopefully, it will make the rounds and make a difference in others lives.
Thiamine Deficiency Disease, Dysautonomia, and High Calorie Malnutrition
This article has a 30% discount code. It's still expensive, but I plan to let my docs borrow it after I am finished. Hopefully, it will make the rounds and make a difference in others lives.
Asklipia
Senior Member
- Messages
- 999
@JasonUT I have been sick from around 1992 or so, just after the war in Iraq, this is now 25 years. I tried all kinds of things, mainly trying all I knew to get healthier generally, not targeting anything in particular, since I did not know what was wrong with me. Some were successful enough and helped me to go on with my life in a reduced way but still enjoyable.
Doctors were no help unfortunately. I got a lot of sympathy but not much else. At least nobody prescribed stuff that would have harmed me. Thanks God for that!
When I started with thiamine supplementation I realized than in fact I had been thiamine deficient all my life (born in 1951), and that the very bad times I had had episodically before 1992 were due to thiamine deficiency undiagnosed for years.
At the moment I am fully functional. But I am surprised to see some of my former limitations being lifted away, dating from childhood.
So I am still on thiamine to see what else it can fix, and I try to convey my experiences to others as a parting gift when I go.
Be well!
And thank you for posting so generously
Asklipia
EDIT : my house is full of guests, no concentration to read Lonsdale's book. I am glad you bought it, it is really interesting and will help in a BIG way I think. Sorry I could not write more about it yet.
Doctors were no help unfortunately. I got a lot of sympathy but not much else. At least nobody prescribed stuff that would have harmed me. Thanks God for that!
When I started with thiamine supplementation I realized than in fact I had been thiamine deficient all my life (born in 1951), and that the very bad times I had had episodically before 1992 were due to thiamine deficiency undiagnosed for years.
At the moment I am fully functional. But I am surprised to see some of my former limitations being lifted away, dating from childhood.
So I am still on thiamine to see what else it can fix, and I try to convey my experiences to others as a parting gift when I go.
Be well!
And thank you for posting so generously
Asklipia
EDIT : my house is full of guests, no concentration to read Lonsdale's book. I am glad you bought it, it is really interesting and will help in a BIG way I think. Sorry I could not write more about it yet.
Last edited:
Asklipia
Senior Member
- Messages
- 999
Now I suspect that the crash was due to the fact that we had been taking high doses of Thiamine for quite a while, and that the presence of the folate has blocked it from being used.Ingredients of Alinamin Ex Plus here.
I am aware that Takeda has a new formulation, called Alinamin Ex Gold. Ingredients of Alinamin Ex Gold here.
Basically, the new Gold formulation replaces cyanocobalamin with mecobalamin, B5 (calcium pantothenate) with B9 (folic acid), B6 with Pyridoxal phosphate hydrate.
Well here is the sequel to this post as promised: last week we ran out of Alinamin Ex Plus and replaced it with Alinamin Ex Gold. We were only taking one pill per day, which is 1/3 of the dose, together with a bunch of the other thiamine supplements. After 3 days we both had a big crash, on only 0.33 mg folic acid per day. That is a total of 1 mg folic acid. It took us two days to recover completely.
FFP

Maybe what happened to @NotThisGuy
So for the moment I am not sure that Folate inhibits Thiamine uptake, we must have adequate levels by now, but it most probably blocks its effect.
@Asklipia
Does this suggest that symptoms would randomly subside with time? Did you observe any rhyme or reason to the healing process?
Thiamine and Niacin are definitely causing something in me. I feel it in me every time I take it. It almost feels like a drug. The hard part is deciphering what is happening. Some symptoms seem to be slowly subsiding, but other symptoms seem to flare randomly. Is the flare the "paradox" of healing? It's so confusing and can be incredibly discouraging when a flare happens.
...But I am surprised to see some of my former limitations being lifted away, dating from childhood. So I am still on thiamine to see what else it can fix, and I try to convey my experiences to others as a parting gift when I go...
Does this suggest that symptoms would randomly subside with time? Did you observe any rhyme or reason to the healing process?
Thiamine and Niacin are definitely causing something in me. I feel it in me every time I take it. It almost feels like a drug. The hard part is deciphering what is happening. Some symptoms seem to be slowly subsiding, but other symptoms seem to flare randomly. Is the flare the "paradox" of healing? It's so confusing and can be incredibly discouraging when a flare happens.
Asklipia
Senior Member
- Messages
- 999
I can feel a progression towards better and better function. It started with more strength in legs, then better sleep, then even better mood with crazy laughing fits, then more sex drive, then more imagination etc.... I don't know what lies in store!@Asklipia
Does this suggest that symptoms would randomly subside with time? Did you observe any rhyme or reason to the healing process?
Interesting to note : more and more memories of what it used to feel like being me, dating further and further in time. Same thing for my husband.
I suppose it could be. I could also be that you are doing something else at that moment that does not allow for the flow of healing. When things get a bit difficult, I try to sleep.Is the flare the "paradox" of healing? It's so confusing and can be incredibly discouraging when a flare happens.
I have noticed changes in food preferences, and not the same from day to day. I try to follow this exactly, because I suppose the body is asking.
I suspect that at least part of the flares happen because I do/eat something contrary to the healing. Maybe folates? It is worth noting down exactly the folates ingested to see if there is an influence.
However, better flares and healing rather than no healing at all! I have stopped worrying about my health, for the first time in at VERY LONG TIME. Maybe twenty years ago I would not have even noticed these flares!
Be well!
Chocolove
Tournament of the Phoenix - Rise Again
- Messages
- 548
@Asklipia @JasonUT
The Alinamin Ex Gold went to the active form of B 6 - Pyridoxal phosphate hydrate. One can get damage from too much B 6. Active forms of B vitamins, (particularly Methylfolate) are well known in PR for causing crashes. Perhaps the active form of B 6 is at issue?
http://forums.phoenixrising.me/index.php?threads/vitamin-b6-safe-dosage.32797/
It may be better to supply the B vitamins in a less active form so that the body can break it down to supply as needed rather than dumping a whole lot of active in at once... thereby avoiding a crash. Assuming of course the body has no problem breaking it down.
Asklipia said: ↑
Ingredients of Alinamin Ex Plus here.
I am aware that Takeda has a new formulation, called Alinamin Ex Gold. Ingredients of Alinamin Ex Gold here.
Basically, the new Gold formulation replaces cyanocobalamin with mecobalamin, B5 (calcium pantothenate) with B9 (folic acid), B6 with Pyridoxal phosphate hydrate.
Click to expand...
Well here is the sequel to this post as promised: last week we ran out of Alinamin Ex Plus and replaced it with Alinamin Ex Gold. We were only taking one pill per day, which is 1/3 of the dose, together with a bunch of the other thiamine supplements. After 3 days we both had a big crash, on only 0.33 mg folic acid per day. That is a total of 1 mg folic acid. It took us two days to recover completely.
The Alinamin Ex Gold went to the active form of B 6 - Pyridoxal phosphate hydrate. One can get damage from too much B 6. Active forms of B vitamins, (particularly Methylfolate) are well known in PR for causing crashes. Perhaps the active form of B 6 is at issue?
http://forums.phoenixrising.me/index.php?threads/vitamin-b6-safe-dosage.32797/
It may be better to supply the B vitamins in a less active form so that the body can break it down to supply as needed rather than dumping a whole lot of active in at once... thereby avoiding a crash. Assuming of course the body has no problem breaking it down.
Last edited:
Asklipia
Senior Member
- Messages
- 999
`
This came to 20 mg Pyridoxal phosphate per day. Since we take with no problem 25 mg sublingual from time to time I don't think the problem lies there.
