I started a thread a while ago on the Psychiatric view of ME/CFS
http://forums.phoenixrising.me/index.php?threads/the-psychiatric-view-of-me-cfs-what-is-it.1309/
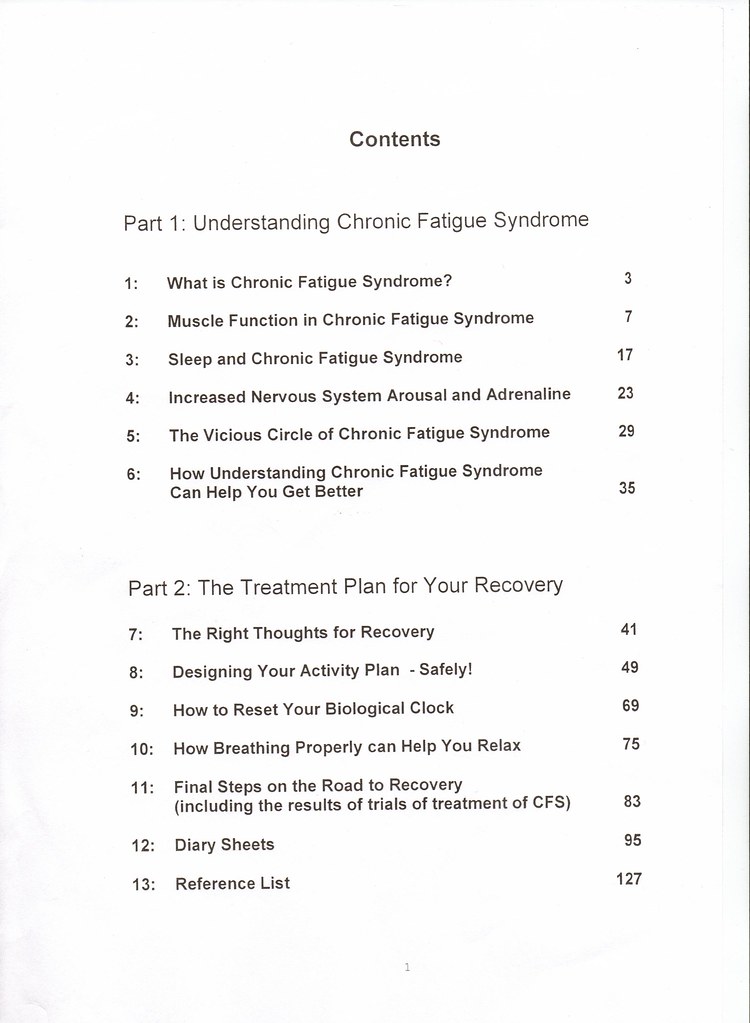
I thought that it would be useful to give a practical example of how these views influence patient care and medical practice on the ground. I have a copy of written information which is given to patients who attend the Liverpool CF/CFS clinic in the UK. At least some of this information is being used in at least one other UK CFS clinic (and was given to a patient there in the last 9 months).
There is a long booklet, a shorter handout which has pretty much the same information summarised, and other information, such as work sheets for the CBT sessions.
The handout also says:
So it is useful to see the sort of information patients are given on this (and very likely similar) trials. Pauline Powells name is on the front page of this document (more on her below). It is dated 2004. Im (not sure why there is a date anomaly, but maybe they just added to it or made minor alterations??).
The information reflects the biopsychosocial, or psychiatric, view of ME/CFS. They argue that ME/CFS is caused by deconditioning, stress (which includes fear of symptoms, and fear that you might have a serious disease) and poor sleep quality from poor sleep hygiene. They think the sleep problems we have are caused by the patient's own bad habits, and that these problems are correctable mostly through behavioural methods. Personality style is also a factor according to them.
These are a few quotes to give you the flavour of the information patients are given:
And
The documents give the impression that, because ME/CFS is caused by deconditioning, stress, and poor sleeping habits, patients have the power to correct these and bring about their own recovery. They go on, and on, and on, about Recovery in the document, as if it is this definitely achievable thing.
I have a funny story about this clinic and recovery. I have heard that as part of the programme people who had previously been on the programme, who were now said to be recovered (by those running the programme), were brought in to meet with patients who were currently the programme. But after talking to them, the patients currently doing the programme realised that these "recovered" patients, were not in fact recovered at all!!
[Please bear with me as it is going take me a while, and quite a few messages, to upload what I have written on this]
http://forums.phoenixrising.me/index.php?threads/the-psychiatric-view-of-me-cfs-what-is-it.1309/
I thought that it would be useful to give a practical example of how these views influence patient care and medical practice on the ground. I have a copy of written information which is given to patients who attend the Liverpool CF/CFS clinic in the UK. At least some of this information is being used in at least one other UK CFS clinic (and was given to a patient there in the last 9 months).
There is a long booklet, a shorter handout which has pretty much the same information summarised, and other information, such as work sheets for the CBT sessions.
The handout also says:
This booklet was part of the randomised controlled trial of patient education to encourage graded exercise in chronic fatigue syndrome (Powell et al. 2001) (p91)
So it is useful to see the sort of information patients are given on this (and very likely similar) trials. Pauline Powells name is on the front page of this document (more on her below). It is dated 2004. Im (not sure why there is a date anomaly, but maybe they just added to it or made minor alterations??).
The information reflects the biopsychosocial, or psychiatric, view of ME/CFS. They argue that ME/CFS is caused by deconditioning, stress (which includes fear of symptoms, and fear that you might have a serious disease) and poor sleep quality from poor sleep hygiene. They think the sleep problems we have are caused by the patient's own bad habits, and that these problems are correctable mostly through behavioural methods. Personality style is also a factor according to them.
These are a few quotes to give you the flavour of the information patients are given:
We now know from the medical research:
There is no persistent virus, no muscle disease or damage
There is no hidden disease (p49)
And
Your thoughts about these symptoms are very important.
If you
Fear the symptoms
Misinterpret the symptoms as signs of disease or relapse
Monitor the symptoms
Feel frustration with the symptoms & limitations in lifestyle
this will cause further nervous system arousal with more symptoms
that can perpetuate the condition.
Consequently, controlling activities controls the levels of symptoms (p 5, short booklet)
The documents give the impression that, because ME/CFS is caused by deconditioning, stress, and poor sleeping habits, patients have the power to correct these and bring about their own recovery. They go on, and on, and on, about Recovery in the document, as if it is this definitely achievable thing.
I have a funny story about this clinic and recovery. I have heard that as part of the programme people who had previously been on the programme, who were now said to be recovered (by those running the programme), were brought in to meet with patients who were currently the programme. But after talking to them, the patients currently doing the programme realised that these "recovered" patients, were not in fact recovered at all!!
[Please bear with me as it is going take me a while, and quite a few messages, to upload what I have written on this]