GlassCannonLife
Senior Member
- Messages
- 819
More details on microclot detection via light microscopy. Claim that only a blood smear is needed. I sort of doubt that as it would be hard to see the microclots among the RBCs, platelets, & other cells. Pertorius used Platelet Free Plasma (PFP), which is plasma that's been centrifuged twice. A smear of PFP would be clearer, I'd think.
View attachment 45973
One Long Covid patient, who is a doctor, discovered microclots in here blood using a light microscope. She is a dermatologist, so you'd think she'd definitely have a microscope in her office.
View attachment 45975
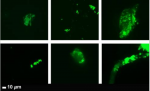
She describes her procedure on how she detected them here. At only 40x (I assume x10 w/ eye piece, so 400x total), a child's microscope or cheapest microscope on amazon for $150 should be able to see that. Maybe even those digital ones for $50.
View attachment 45978
Images of her results, and description of procedure:
View attachment 45977
That's interesting! Shame I can't work anymore, we had all of these things in the lab.
A 4x objective is pretty common so I don't know if it's necessarily 400x vs actually 10x eye piece and 4x objective. We had some small bench microscopes that would have 2.5, 4, 10, and 25 IIRC.