PoTS and ME/CFS: Basic information and links from the MEA:
1 The MEA also has a brand new information leaflet covering all aspects of PoTS in relation to ME/CFS:
http://www.meassociation.org.uk/shop/management-leaflets/orthostatic-intolerance/
as well as a leaflet covering the management of orthostatic intolerance:
http://www.meassociation.org.uk/shop/management-leaflets/orthostatic-intolerance-2/
2 Information on POTS from the MEA purple book - clinical assessment section:
Postural orthostatic tachycardia syndrome (PoTS) sometimes forms part of ANS dysfunction in ME/CFS.
PoTs is defined as symptoms of orthostatic intolerance associated with an increase of heart rate from supine to upright position of > 30 beats per minute (or 40 beats per minute in the 12-19 year age group) or with a heart rate of > 120 beats per minute on standing, can occur in ME/CFS (Hoad
et al 2008; Kavi
et al 2016).
In the recent British Journal of Cardiology review of patients with PoTS and their experience of healthcare in the UK, Kavi
et al (2016) found that 81% of respondents were between the ages of 18 and 49 years and 92% were female.
The most common symptoms at presentation were fatigue (91%), light-headedness, dizziness or presyncope (90%) and palpitations (86%). Syncope or blackouts were experienced by 58%.
Other commonly presenting symptoms (in over 40%) included difficulty thinking (often described as brain fog), physical weakness, visual disturbances, breathlessness, vertigo, shakiness, chest pain, sweating, bloating, symptoms of anxiety, poor sleep, daily headache, acrocyanosis (purple-blue discolouration of hands and lower limbs), tingling in peripheries, nausea, abdominal pain, heat and exercise intolerance and ‘coat hanger’ pain (thought to be due to ischaemia of neck and shoulder muscles).
Clinical evaluation should therefore include a response to standing.
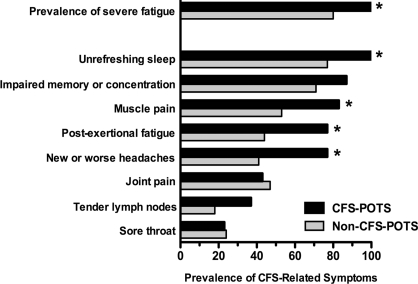
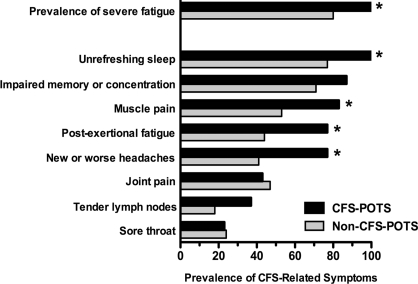
Research aimed at characterising ME/CFS patients with or without PoTS found that those with PoTS were younger, less fatigued, less depressed and had reduced daytime somnolence (Lewis
et al 2013a). They also had greater orthostatic intolerance and autonomic dysfunction. Those with PoTS may require further investigation and consideration for therapy to control heart rate (Lewis
et al 2013a).
Further evidence relating to the important subgroup of ME/CFS patients who also have PoTS comes from Nijs and Ickmans (2013).
For a review of PoTS, see Benarroch (2012) and Kavi
et al (2016).
NB: In patients presenting with chronic fatigue and/or orthostatic intolerance, low ferritin levels and hypovitaminosis D may be present, especially in those with postural tachycardia (Antiel
et al 2011).
3 Information on symptoms and diagnosis of PoTs from the new MEA information leaflet
Why does PoTS sometimes affect people with ME/CFS?
PoTS can affect people with ME/CFS, especially those in younger age groups and at the more severe end of the spectrum.
This is because the ANS is commonly involved in ME/CFS – where the malfunction can cause what is called orthostatic intolerance (difficulty in remaining upright – as in PoTS) and cold hands and feet. The ANS also affects bowel and bladder control and may therefore cause irritable bowel type symptoms and ‘irritable bladder’ symptoms.
Primary PoTS and overlap with other conditions
Primary PoTS often has an abrupt onset and may follow acute infections, immunisations, surgery, pregnancy, or trauma – all of which can trigger ME/CFS.
As with ME/CFS, there is evidence of an autoimmune component and there is a genetic component in some cases.
PoTS is also more common in people who have hypermobile joints (which can also overlap with ME/CFS), people who are deconditioned after prolonged bed rest, diabetes, sarcoidosis, Sjogren’s syndrome, SLE/lupus, antiphospholipid (Hughes) syndrome, and mast cell activation disorder - which should be checke for this if flushing and allergies are present.
What are the diagnostic symptoms and signs?
Characteristic symptoms, which occur on standing and are normally relieved by lying down, include:
·fatigue or weakness (91%)
·palpitations or awareness of the heart beating (86%)
·dizziness (90%)
·feeling light-headed, pre-syncope/feeling faint (90%)
·sometimes actually fainting/syncope (58%), or having a transient loss of consciousness
Percentages are taken from a PoTS UK patient survey.
Other common symptoms, which occur in up to 40% of cases, include:
·nausea and other irritable bowel type symptoms
·headaches – which may be caused by lack of blood flow to the brain,
·sleep disturbance
·shortness of breath and chest pain
·visual disturbances – including blurring
·‘brain fog’/cognitive dysfunction – as occurs in ME/CFS
·‘coat hanger pain’ - which is thought to be due to poor blood supply to muscles around the neck and shoulder
Acrocyanosis – a puffy bluish discolouration of the hands and feet that is caused by blood pooling in the veins occurs in around 50% of cases.
Symptoms are often described as being more prominent on rising after waking up. They are frequently exacerbated by standing up too quickly, heat, some types of food or large meals, alcohol and stress. They are often exacerbated during infections and may be worse during menstruation.
For some people, the disability caused by PoTS is considerable, especially when this is added to the health problems caused by ME/CFS. Patient evidence collected by PoTS UK indicates that 23% are wheelchair users and 37% are unable to work. Although severely incapacitated, PoTS patients often look well.
Slide of acrocyanosis:
http://mddk.com/wp-content/uploads/2015/11/acrocyanosis-pictures-2.jpg
How is PoTS diagnosed?
A diagnosis of PoTS is based on the characteristic symptoms and what is called a 10 minute active stand test and/or a tilt table test.
The Active Stand Test: Under careful supervision, heart rate and blood pressure are measured after resting/lying down for ten minutes, then immediately upon standing still (unsupported with hands by sides) and after 2, 5 and 10 minutes. This test may bring on symptoms of PoTS and some people may faint. If the result is uncertain the test can be repeated on another occasion.
Head-Up Tilt Table Test: This involves lying on a table that can be tilted to an angle of 60 to 70 degrees in a quiet, dimly lit, temperature controlled room. Blood pressure and heart rate are recorded in a continuous manner. After a period of 5 to 20 minutes of lying flat, the table is tilted. Although a diagnosis of PoTS should be made by an increase in heart rate of 30 beats per minute within the first 10 minutes, this upright position can last between 10 and 45 minutes.
The patient will be asked how they are feeling during the test, so symptoms can be matched with heart rate and blood pressure.
The test will end if your blood pressure becomes too low, satisfactory results have been obtained, or the maximum time has elapsed.
If facilities are available, some patients are tilted after a carbohydrate drink (liquid meal challenge), exercise or heat.
Serum catecoholamines should be checked in supine and upright positions, especially if a hyperadrenergic form of PoTS is suspected.
A heart rhythm test/electrocardiogram test should also be arranged to exclude heart problems that can cause a tachycardia as well (eg inappropriate sinus tachycardia) and thyroid function tests.
Other cardiac/heart tests – eg 24 hour heart rate and blood pressure monitoring, echocardiogram, autonomic function screening tests - may be required in more complicated cases.
Unfortunately, many doctors still know little or almost nothing about how to diagnose PoTS and how to manage it. As a result, many people with PoTS are left undiagnosed, may even be misdiagnosed as having anxiety, panic attacks or hypochondriasis, or be labeled as ‘heart-sink’ patients.
Dr Charles Shepherd
Hon Medical Adviser, MEA