> /If you don't rule out such ordinary problems how on Earth can you
> diagnose something like a channelopathy? /
Exactly. Even the researchers and advanced diagnosticians do not behave
in a satisfactory way.
The reason they have trouble is sad but straightforward. They're
imbeciles and don't read. They also don't look for or follow the key
flowcharts -- not even the main diagnosticians.
They seem to just follow a "seat-of-the-pants" method, at least, for me.
In my case, I think my documented anesthesia history, arrhythmia records
and other autonomic responses made it "obvious" to them that I had PP.
When I wanted them to give me the
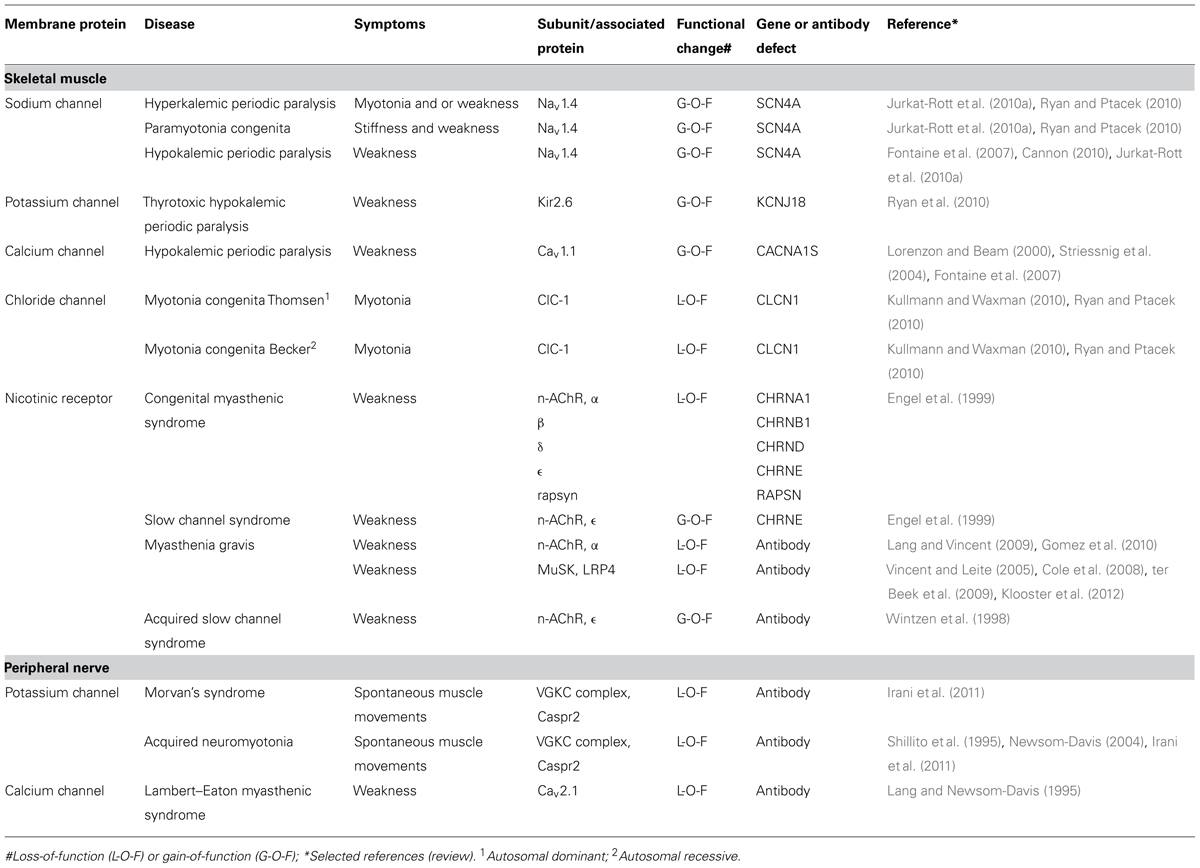
CMAP test (which is one of the more
definitive tests), I was told that it was a tedious test that would take
him all afternoon and he didn't want to do it -- and he said it was
obvious to him that I had PP anyway. I was not pleased...
A person can also add
TTKG, since the TTKG test helps determine if there
is a loss of potassium or a shift, or they could add CMAP.