THIS IS A GREAT POST and I want to add to it that CHOLANGITIS is clogged bile ducts !! and it can results in antibodies to the E2 complex of the PDC . I have been researching this for some time -- because I had oxalate toxicity and severe gall bladder issues in 2013. I feel much better now but need to be very vigilant to make sure I avoid foods which inhibit bile production and I need to eat soluble fiber to bind the thick sludgy bile and force it to be excreted.
I think this is made much worse by high oxalate diet -- because oxalates inhibit bile production ! CLEVELAND CLINIC Dr Aaron Miller gave a presentation to the TLO oxalate group on this in Nov 2023. You can find this on my timeline in facebook Search for youtube and Cleveland Clinic and oxalates under my profile. I dont know if I can post a link here .
but I want you to see this about the E2 unit and cholangitis: "


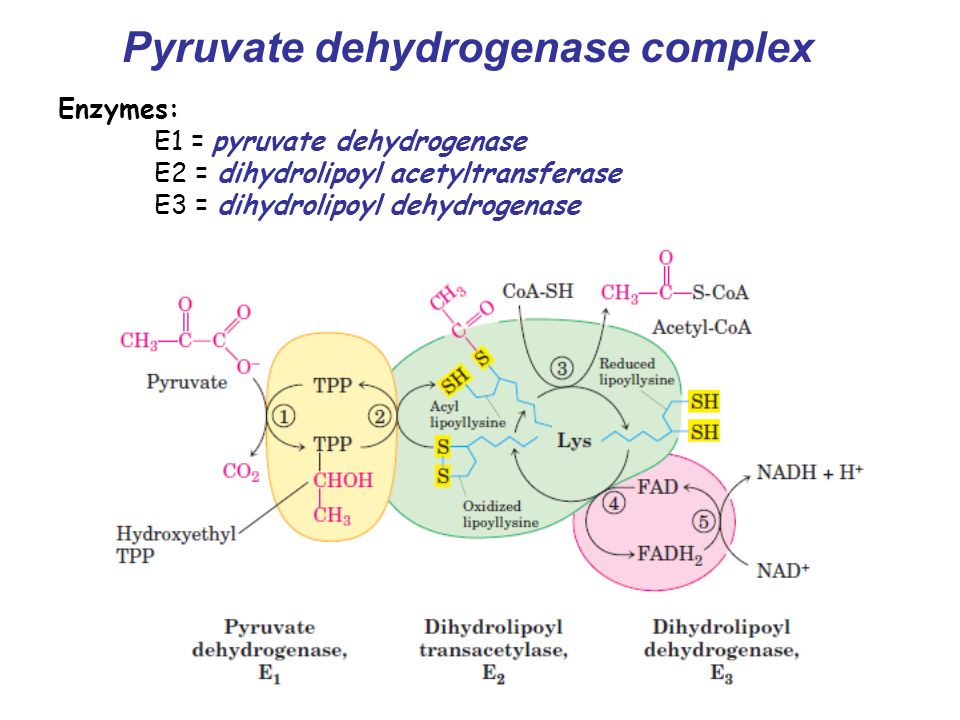
The serologic hallmark of PBC (Primary biliary cholangitis)
in 95%–98% of the patients is the presence of M2 anti-mitochondrial autoantibodies (AMAs)


directed against the


E2 subunit of the


pyruvate dehydrogenase multi-enzyme complex located in the inner membrane of mitochondria. "
"The present case involved a 54-year-old woman who had severe pain on the left side of the TMJ and had a limited mouth interincisal opening (MIO) for the past 6 months.
On clinical examination, we did not observe any facial swelling or asymmetry, and there was no tenderness of the masticatory muscles on palpation.


Maxillary molars were missing bilaterally, and she was wearing an ill-fitted denture

. Her MIO was 16 mm; this interfered with her daily activities, including chewing, talking, yawing,
Result
Biochemical and immunological examination results showed high γ-GTP, ALP, AMA, anti-mitochondrial-M2 (AMA2) antibody, and IgM levels in the peripheral blood sample. AMA2, a specific antibody for PBC, and high IgM levels were detected only in the synovia from the affected side of the TMJ (Table 1).


In our presented case, using immunohistochemistry, we also detected the presence of IL-17-positive cells in the liver with PBC (Fig. 2). Additionally, using RT-PCR, we observed that IL-17 m-RNA levels
Discussion


IL-17-producing CD4 (+) helper T (Th17) cells that have been identified as one of the major pathogenic Th cell populations is the basis of the development of many autoimmune diseases, and IL-23 is known to enhance and stabilize them. [11].
The discovery of the cytokine identity of the IL-17 family and the discovery that IL-23 mediates the proliferation of IL-17 producing T cells led to the discovery of a new subset of Th cells called Th17 cells. Like Th1 and Th2 cells, Th17 cells require…”
https://www.sciencedirect.com/science/article/abs/pii/S2212555818303399