sb4
Senior Member
- Messages
- 1,659
- Location
- United Kingdom
https://sci-hub.tw/10.1016/j.mehy.2019.109260
Apparently this has been discussed before but I missed it last time, so have just caught up. It's a paper from some Norwegian researches that found supplying oxalates in the form of some type of spinach drink, dramatically improved symptoms in some patients. This paper is laying out what they think the mechanism is.
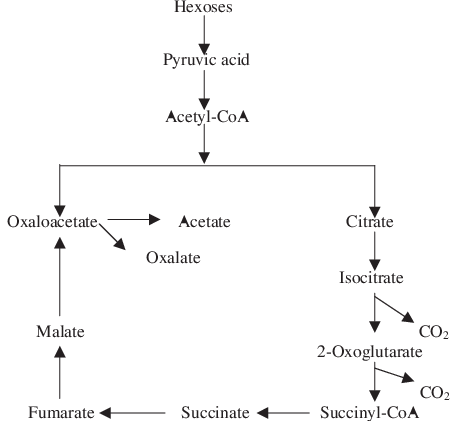
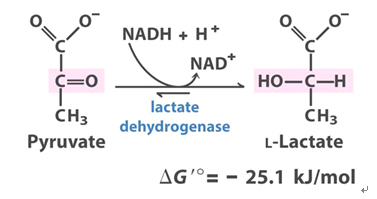
I think these images help to explain what is going on:
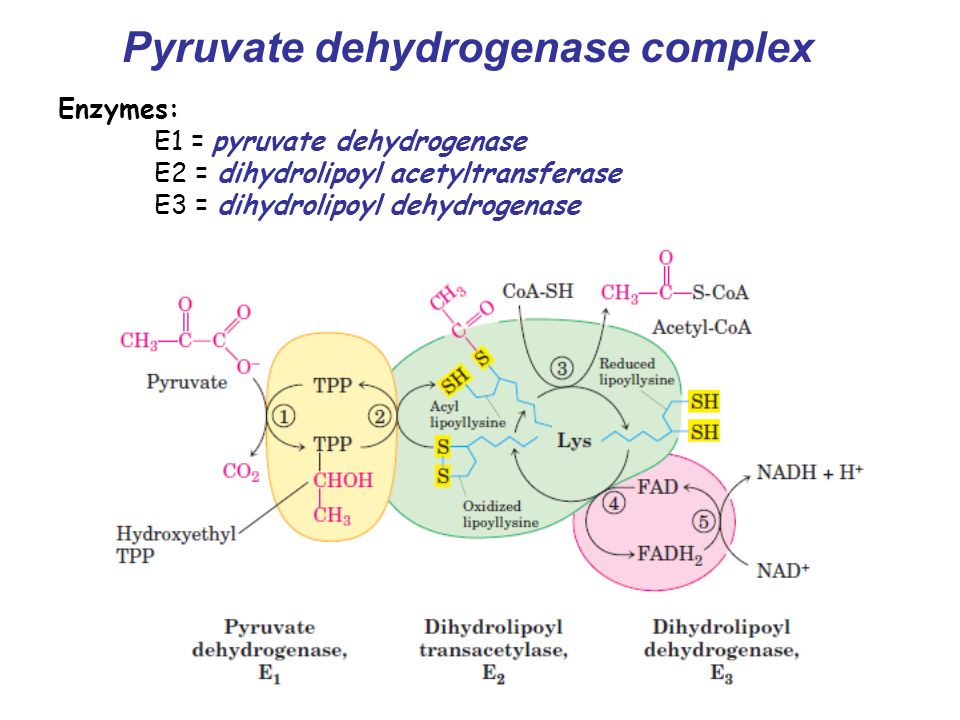

As far as I understand it, they are proposing that something is stopping DHLA (dihydrolipoic acid)[Reduced lipoyllysine] from recycling back into LA (lipoic acid)[Oxidized lipoyllysine]. This causes a backup in the PDC (Pyruvate Dehydrogenase Complex) and Pyruvate does not get transformed into Acetyl-CoA, leaving an energy deficit.
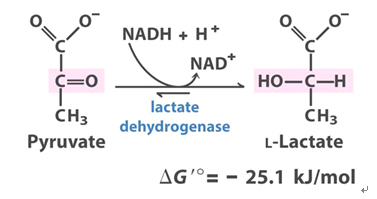
Now is the bit that gets confusing. They say that 2 pyruvate need to enter into the mitochondria and react with PDC for the enzyme to work. This is because one of the pyruvate needs to enter the E1 complex and the other needs to get transformed into lactate, and in the process recycle the NADH+H+ that is generated at the last step of the PDC in the E3 complex.
So in healthy people there apparently is a 1:1 ratio of Pyruvate and Lactate (in the mitochondria?). However, and I am not sure if this is correct, what happens in CFS is the 2 pyruvate enter the mito, one is converted to lactate, and the other stays as pyruvate when it should be converted to Acetyl-CoA. This is because DHLA is not recycling into LA backing up the whole system.
Then I assume the relative lack of Acetyl-CoA causes the mito to ask for more pyruvate or perhaps the left over pyruvate gets turned into Lactate via LDH. This causes a spike in Lactate whenever the cell is mildly stressed or needs to use more energy. I would have though this increased Lactate would be due to pyruvate backlog turning into Lactate in the cytosol in order to replace the missing energy from Acetyl-CoA.
Now they intend to get around this problem using oxalates. As far as I am aware oxalate reverses the conversion of Pyruvate to lactate and of Pyruvate to Oxaloacetate. Since Pyruvate has 3 choices, convert to Lactate, Oxaloacetate, or Acetyl-CoA, perhaps by "inhibiting" the other 2 we can force more Acetyl-CoA. It appears they are advocating doing this in conjuction with providing LA and possibly Riboflaving / Thiamine to try to overcome the DHLA block.
What I have been able to piece together from another thread is that 2 people tried high oxalates (through spinach I believe) and felt better for a short while then worse. However, according to the researches, there where a handful of people they tested this drink on who achieved remission as long as they kept drinking the drink.
I am particularly interested in this as I have significantly improved my carb tolerance (though it is still not great) by taking MCT oil with carbs. I speculate that the mechanism is via providing cells (/the liver) with so much Acetyl-CoA from the MCTs that pyruvate will ignore PDH and instead go through PC into Oxaloacetate. These researches seem to be presenting a similar mechanism for oxalates.
Systemic Exertion Intolerance Disease (SEID) or myalgic encephalomyelitis (ME) or chronic fatigue syndrome (CFS) has an unknown aetiology, with no known treatment and a prevalence of approximately 22 million individuals (2%) in Western countries. Although strongly suspected, the role of lactate in pathology is unknown, nor has the nature of the two most central symptoms of the condition – post exertional malaise and fatigue. The proposed mechanism of action of pyruvate dehydrogenase complex (PDC) plays a central role in maintaining energy production with cofactors alpha-lipoic acid (LA) and its counterpart dihydrolipoic acid (DHLA), its regeneration suggested as the new rate limiting factor. Decreased DHLA regeneration due to impairment of the E3 subunit or crossover of the swinging arms of the E2 subunit of PDC have been suggested as a cause of ME/CFS/SEID resulting in instantaneous fluctuations in lactate levels and instantaneous offset of the DHLA/LA ratio and defining the condition as an LA deficiency with chronic instantaneous hyperlactataemia with explicit stratification of symptoms. While instantaneous hyperlactataemia has been suggested to account for the PEM, the fatigue was explained by the downregulated throughput of pyruvate and consequently lower production of ATP with the residual enzymatic efficacy of the E3 subunit or crossover of the E2 as a proposed explanation of the fatigue severity. Functional diagnostics and visualization of instantaneous elevations of lactate and DHLA has been suggested. Novel treatment strategies have been implicated to compensate for chronic PDC impairment and hyperlactataemia. This hypothesis potentially influences the current understanding and treatment methods for any type of hyperlactataemia, fatigue, ME/CFS/SEID, and conditions associated with PDC impairment.
Apparently this has been discussed before but I missed it last time, so have just caught up. It's a paper from some Norwegian researches that found supplying oxalates in the form of some type of spinach drink, dramatically improved symptoms in some patients. This paper is laying out what they think the mechanism is.
I think these images help to explain what is going on:
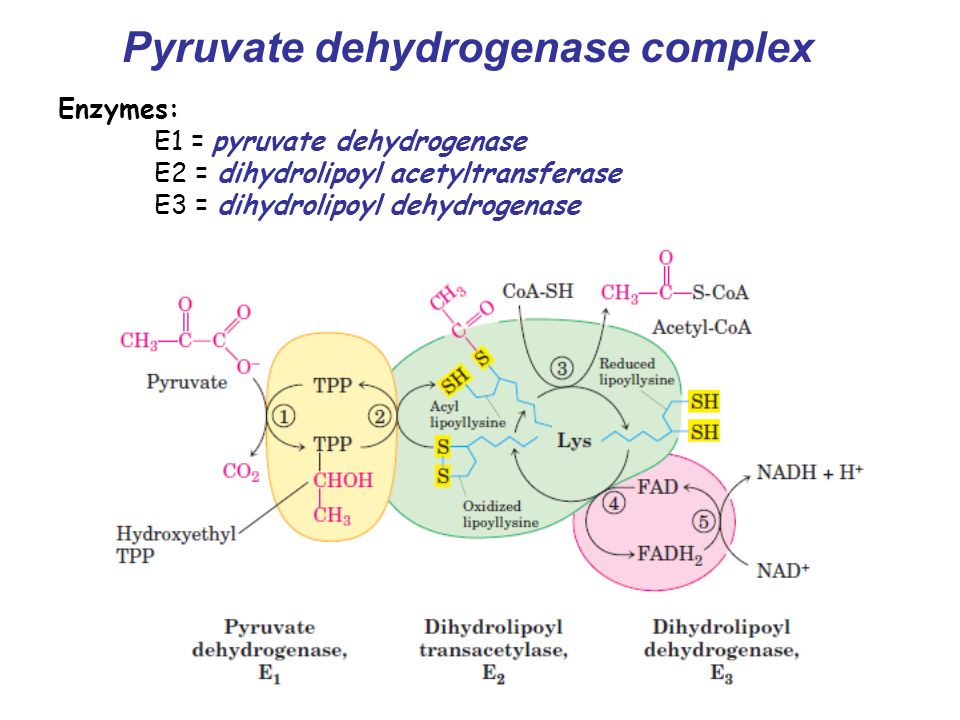

As far as I understand it, they are proposing that something is stopping DHLA (dihydrolipoic acid)[Reduced lipoyllysine] from recycling back into LA (lipoic acid)[Oxidized lipoyllysine]. This causes a backup in the PDC (Pyruvate Dehydrogenase Complex) and Pyruvate does not get transformed into Acetyl-CoA, leaving an energy deficit.
Now is the bit that gets confusing. They say that 2 pyruvate need to enter into the mitochondria and react with PDC for the enzyme to work. This is because one of the pyruvate needs to enter the E1 complex and the other needs to get transformed into lactate, and in the process recycle the NADH+H+ that is generated at the last step of the PDC in the E3 complex.
So in healthy people there apparently is a 1:1 ratio of Pyruvate and Lactate (in the mitochondria?). However, and I am not sure if this is correct, what happens in CFS is the 2 pyruvate enter the mito, one is converted to lactate, and the other stays as pyruvate when it should be converted to Acetyl-CoA. This is because DHLA is not recycling into LA backing up the whole system.
Then I assume the relative lack of Acetyl-CoA causes the mito to ask for more pyruvate or perhaps the left over pyruvate gets turned into Lactate via LDH. This causes a spike in Lactate whenever the cell is mildly stressed or needs to use more energy. I would have though this increased Lactate would be due to pyruvate backlog turning into Lactate in the cytosol in order to replace the missing energy from Acetyl-CoA.
Now they intend to get around this problem using oxalates. As far as I am aware oxalate reverses the conversion of Pyruvate to lactate and of Pyruvate to Oxaloacetate. Since Pyruvate has 3 choices, convert to Lactate, Oxaloacetate, or Acetyl-CoA, perhaps by "inhibiting" the other 2 we can force more Acetyl-CoA. It appears they are advocating doing this in conjuction with providing LA and possibly Riboflaving / Thiamine to try to overcome the DHLA block.
What I have been able to piece together from another thread is that 2 people tried high oxalates (through spinach I believe) and felt better for a short while then worse. However, according to the researches, there where a handful of people they tested this drink on who achieved remission as long as they kept drinking the drink.
I am particularly interested in this as I have significantly improved my carb tolerance (though it is still not great) by taking MCT oil with carbs. I speculate that the mechanism is via providing cells (/the liver) with so much Acetyl-CoA from the MCTs that pyruvate will ignore PDH and instead go through PC into Oxaloacetate. These researches seem to be presenting a similar mechanism for oxalates.