Thanks Shane and Lisa! Shane-I do think that I'll ask for a Holtor monitor. I'm glad you mentioned that. At least that will prove the weird heart stuff (racing heart and flutters, shortness of breath) that I frequently get. Dear goodness, you've been through the ringer! Breaks my heart to read what so many others have had to go through. Lisa-yes, my doc certainly made it clear that he does not believe me, and for now, I am far too worn down to find one who does. I am so happy to have stumbled across this forum. Over the past few years, most of my friends have disappeared and I miss that companionship so badly-now, I feel like I've found it again.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Seizures
- Thread starter JMK
- Start date
sarahg
Admin Assistant
- Messages
- 276
- Location
- Pennsylvania
JMK- welcome and I hope you find all that you need here. be forewarned that the holter monitor may not show anything...or the results may be misinterpreted easily. Might be better to find a new DR. first.
I had to do a holter monitor test (24 hrs) during a time period of frequent chest pains, heart racing, palpitations and dizziness. It came back "normal". the technician that did it (not my normal doctor, but a nurse practitioner in the same complex) said of the results "there were some abnormalities, but it was normal"
Normal abnormalities? pretty much sums up what we are faced with based on who is reading the results. If I recall correctly, I had a sleep study once that said pretty much the same, verbatim. Your best bet is to find a Dr. who can actually interpret the results.
Anyway, this next part probably won't help you. I have only had one seizure and it was while I was waking up from anesthesia after an abdominal surgery. Apparently a bad reaction to the anesthesia, an absolutely terrifying way to wake up from a surgery.
I had to do a holter monitor test (24 hrs) during a time period of frequent chest pains, heart racing, palpitations and dizziness. It came back "normal". the technician that did it (not my normal doctor, but a nurse practitioner in the same complex) said of the results "there were some abnormalities, but it was normal"
Normal abnormalities? pretty much sums up what we are faced with based on who is reading the results. If I recall correctly, I had a sleep study once that said pretty much the same, verbatim. Your best bet is to find a Dr. who can actually interpret the results.
Anyway, this next part probably won't help you. I have only had one seizure and it was while I was waking up from anesthesia after an abdominal surgery. Apparently a bad reaction to the anesthesia, an absolutely terrifying way to wake up from a surgery.
Getting the right Doc
I do have to say, my cardiologist is great. He does not completely understand everything that is going on but he is very open to looking and he is convinced based upon all that he sees that there is an autonomic issue. He has repeatedly encouraged me to keep looking for the root cause. He's also the chief of cardiology of a large regional hospital system. A unique situation. I had a good friend that is a chief cardiologist at another local hospital and he agrees with my assessment of this doc. I got into see him because I called the Heart Clinic after having been dismissed by one of his underlings. My present cardiologist just happened to have a cancellation that afternoon and I was experiencing chest pain.
I agree with sarahg - don't settle for a doc that doesn't believe you. They won't look for, and therefore they won't notice, subtle patterns that are right in front of them. Then you'll have one more "she's a hypochondriac" note in your records to over come. More harm than good. My Holter didn't provide an answer, it raised more questions. It took my doctor recognizing that things didn't look quite right to follow up (like why was your pulse 120 bpm at 2 am - I was asleep).
Shane
I do have to say, my cardiologist is great. He does not completely understand everything that is going on but he is very open to looking and he is convinced based upon all that he sees that there is an autonomic issue. He has repeatedly encouraged me to keep looking for the root cause. He's also the chief of cardiology of a large regional hospital system. A unique situation. I had a good friend that is a chief cardiologist at another local hospital and he agrees with my assessment of this doc. I got into see him because I called the Heart Clinic after having been dismissed by one of his underlings. My present cardiologist just happened to have a cancellation that afternoon and I was experiencing chest pain.
I agree with sarahg - don't settle for a doc that doesn't believe you. They won't look for, and therefore they won't notice, subtle patterns that are right in front of them. Then you'll have one more "she's a hypochondriac" note in your records to over come. More harm than good. My Holter didn't provide an answer, it raised more questions. It took my doctor recognizing that things didn't look quite right to follow up (like why was your pulse 120 bpm at 2 am - I was asleep).
Shane
Holter Monitors and Home BP
Hi Athene,
I could not agree more on every point.
Luckily, my Internist and cardiologist are great about viewing things in context. I have cardiac instability meaning I have huge swings in BP and HR (even to some degree while on ace inhibitors and beta blockers).
I have periods where 150 mg of metoprolol (a beta blocker) is just enough to keep my HR down to 70-75 bpm. Then overnight my HR will drop to 35 bpm and I have to significantly reduce or even stop my beta blockers immediately. When I am on a low dose of beta blockers I don't go anywhere without enough to bring my HR down should it spike.
Before heart meds my HR was usually very high (spikes of 100 -120 bpm or so at rest - sometimes even in my sleep - Holter monitor) but there were times when it would drop to 25 bpm for just a few minutes.
For myself, the meds control the extremes and do not address the underlying neural issues (I have talked with my doc about a pace maker because of the drops but they aren't frequent enough and don't last long enough to go there now) I do take my HR and BP (using a home monitor) when I wake and before bed (I don't adjust meds for small shifts in BP but I do when I have a larger sustained shift and only after talking with my docs).
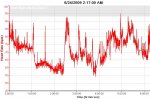
This might sound a bit crude but one way I got everyone's attention was with a sports HR monitor (Garmin) that saves HR readings for up to 7 hours and the readings can be downloaded and graphed on my computer. I printed out 24 hours worth of readings and my cardiologist immediately ordered the monitor.

It was clear from these recordings that my HR was spiking every 15-30 minutes (the above was taken while I was asleep - the spikes would repeatedly wake me as my chest would be POUNDING).
I'm fortunate to be seeing a very good cardiologist but I know he's consulting with his electrophysiology lab. I've had three 24 hour Holter tests, all eight lead with lots of shaving. This probably isn't an issue for you - but I'm now asking the nurse who applies the electrodes to that if she needs to shave a patch that she do so in the shape of a heart. It definitely lightens the mood.
One last point - I was talking with the nurse doing my last EKG and she said her husband had recently suffered a heart attack and now he just can't stop talking about it - "he's telling complete strangers while we're out for dinner." I also have a good friend (Air Force pilot) who had a heart attack just this past Monday night.
I suggested to that nurse (as well as my friend's wife) that there is not much in life that is as unsettling as having heart issues. You've spent your life blissfully unaware of it and now you wonder if you can count on it to keep doing its thing. The nurse agreed. She said that she can tell when someone comes in if they've had previous issues, "it changes them." But as Athene and I both would attest, it is manageable with the right treatment.
Take care of yourself and as hard as it is, try to stay as calm about this as you can. It may also help the doc take you more seriously (not that its right for you to need to worry about him).
eg. I was once told my pulse of 40 bpm during the night was "normal" Ha ha ha!!! That's only normal if you are an olympic long distance runner, not if you are a middle aged biddy who can't get up a flight of stairs without sitting down half way!!! They don't relate the "normal parameters" to the actual person they are dealing with, is my point.
Two things: You need an electrophysiologist - regular cardiologists are bullshitting if they pretend they can interpret a Holter properly. It is a specialised field in itself.
Second - You need an eight lead Holter. Fewer leads and you miss vital info. Some Holters only have 2 leads!!! An electrophysiologist would never give you that!
Finally, Shane, OMG what an awful thing you have suffered! I am glad to hear you are over it. JMK, I guess regular monitoring of your blood pressure is something you could easily do with one of those home gadgets??
Hi Athene,
I could not agree more on every point.
Luckily, my Internist and cardiologist are great about viewing things in context. I have cardiac instability meaning I have huge swings in BP and HR (even to some degree while on ace inhibitors and beta blockers).
I have periods where 150 mg of metoprolol (a beta blocker) is just enough to keep my HR down to 70-75 bpm. Then overnight my HR will drop to 35 bpm and I have to significantly reduce or even stop my beta blockers immediately. When I am on a low dose of beta blockers I don't go anywhere without enough to bring my HR down should it spike.
Before heart meds my HR was usually very high (spikes of 100 -120 bpm or so at rest - sometimes even in my sleep - Holter monitor) but there were times when it would drop to 25 bpm for just a few minutes.
For myself, the meds control the extremes and do not address the underlying neural issues (I have talked with my doc about a pace maker because of the drops but they aren't frequent enough and don't last long enough to go there now) I do take my HR and BP (using a home monitor) when I wake and before bed (I don't adjust meds for small shifts in BP but I do when I have a larger sustained shift and only after talking with my docs).
This might sound a bit crude but one way I got everyone's attention was with a sports HR monitor (Garmin) that saves HR readings for up to 7 hours and the readings can be downloaded and graphed on my computer. I printed out 24 hours worth of readings and my cardiologist immediately ordered the monitor.
It was clear from these recordings that my HR was spiking every 15-30 minutes (the above was taken while I was asleep - the spikes would repeatedly wake me as my chest would be POUNDING).
I'm fortunate to be seeing a very good cardiologist but I know he's consulting with his electrophysiology lab. I've had three 24 hour Holter tests, all eight lead with lots of shaving. This probably isn't an issue for you - but I'm now asking the nurse who applies the electrodes to that if she needs to shave a patch that she do so in the shape of a heart. It definitely lightens the mood.
One last point - I was talking with the nurse doing my last EKG and she said her husband had recently suffered a heart attack and now he just can't stop talking about it - "he's telling complete strangers while we're out for dinner." I also have a good friend (Air Force pilot) who had a heart attack just this past Monday night.
I suggested to that nurse (as well as my friend's wife) that there is not much in life that is as unsettling as having heart issues. You've spent your life blissfully unaware of it and now you wonder if you can count on it to keep doing its thing. The nurse agreed. She said that she can tell when someone comes in if they've had previous issues, "it changes them." But as Athene and I both would attest, it is manageable with the right treatment.
Take care of yourself and as hard as it is, try to stay as calm about this as you can. It may also help the doc take you more seriously (not that its right for you to need to worry about him).
Attachments
Dr. Yes
Shame on You
- Messages
- 868
Seizure-related?
Hi all,
Very interesting discussion here..I had just recently been wondering about "low-level" seizure activity that I believe Cheney and others have spoken of..
A few of us have been wondering about the possible connection between mild seizure activity and weird, intense perceptual anomalies similar to depersonalization/ derealization (this discussed, oddly, on the Buddhism thread). These episodes seem to last for a certain amount of time and then disappear, and do not seem to correlate clearly to psychological factors. The first one I experienced was during my first night in an old apartment, which interests me about the toxic mold issue Khaly brought up. The second "phase" of my illness was accompanied by much more of this symptom, and began with a worsening of allergies (I have moderate allergies to common molds; don't know about Aspergillus niger, but I used to see spots of black mold on the walls in some rooms...).
This symptom was most often triggered by excessive sensory stimulation, usually by very vivid TV shows (not as much of a problem on a black-and-white, oddly).
Athene, does this fit the picture of any of the forms of seizure or seizure-related symptoms you've researched (such as the 'auras')?
Also..does anyone know how in the US you can get a cerebral perfusion scan of any sort covered by insurance?
Hi all,
Very interesting discussion here..I had just recently been wondering about "low-level" seizure activity that I believe Cheney and others have spoken of..
A few of us have been wondering about the possible connection between mild seizure activity and weird, intense perceptual anomalies similar to depersonalization/ derealization (this discussed, oddly, on the Buddhism thread). These episodes seem to last for a certain amount of time and then disappear, and do not seem to correlate clearly to psychological factors. The first one I experienced was during my first night in an old apartment, which interests me about the toxic mold issue Khaly brought up. The second "phase" of my illness was accompanied by much more of this symptom, and began with a worsening of allergies (I have moderate allergies to common molds; don't know about Aspergillus niger, but I used to see spots of black mold on the walls in some rooms...).
This symptom was most often triggered by excessive sensory stimulation, usually by very vivid TV shows (not as much of a problem on a black-and-white, oddly).
Athene, does this fit the picture of any of the forms of seizure or seizure-related symptoms you've researched (such as the 'auras')?
Also..does anyone know how in the US you can get a cerebral perfusion scan of any sort covered by insurance?
Cheney and Heart Issues as a Buhdist Awakening
Athene, Sorry to hear about your mom. Thanks for the info on Dr. Cheney. I know that my cardiologist would be open to anything that helps to explain what's has been going on and help to treat it. As I have said before, I really like my cardio - he's chief of cardiology at a very well regarded heart center, very bright, open minded, curious and best of all, caring. That said, in the middle of this his strong advice was to "keep looking for an answer, you cannot afford to wait, your heart is strong and that's a good thing, we're controlling this to a degree but something is driving your neural signals and it seems to be outside of my area of expertise. Please keep me posted."
I've had so many ultrasounds and x-rays in the last 12 months that we really haven't had a chance to get on a regular schedule but I suspect that will be the case. My next appt with him is just after the new year. I do have an moderately enlarged left ventricle and a somewhat low ejection fraction.
Before getting sick and during a period of remission I have always been very fit. Lots of long distance cycling, back country skiing, and hiking is probably buying me some time right now.
Again, thank you for the info on Dr. Cheney. Also, Dr. Montoya recognized the pattern immediately and labeled it "cardiovascular instability resulting from autonomic neural issues." In light of all the infectious stuff going on, that seems right on to me.
Dr. Yes,
For myself (and I realize that my experience may not be the same as everyone else), the cardio issues started out mildly and kept on a very steady decline over the course of 3-4 months that left me peering directly into the abyss. Many nights this past summer I took my sleep meds without the least bit of confidence that the meds wouldn't interact with the heart/cerebral vascular/neuro-issues and push me over the edge but I needed sleep. Living like that from April to July definitely put a dent in my old view of reality.
Best to everyone,
Shane
Hiya Shane,
Have you read all of Paul Cheney's research on cardiac issues in CFS? He's explained a lot about fluctuating pulse and bp as well as orthostatic intolerance. I don't know what he says about treatment to control it but it may be worth looking into, in case there is something better than the meds you are on.
My mother has exactly the same issues and she also has an enlarged heart (apparently it gets someting like stretch marks as the muscle weakens) and prolapsed valves because it has such high back pressure inside... which then actually correlates to low peripheral bp. You can have something when the bp in your heart and lungs is excessively high while the bp as measured in your arm is low. Apparently this is rarely diagnosed as it is so rare and also very hard to measure. Somewhat irritatingly I cannot remember the name of it but I'll keep thinking till it comes back to me.
I guess regular ultrasounds and Xrays of your heart would be good idea to keep tabs on the pyhsical structure. I have been told every 6 months - is that what your cardio said?
Athene, Sorry to hear about your mom. Thanks for the info on Dr. Cheney. I know that my cardiologist would be open to anything that helps to explain what's has been going on and help to treat it. As I have said before, I really like my cardio - he's chief of cardiology at a very well regarded heart center, very bright, open minded, curious and best of all, caring. That said, in the middle of this his strong advice was to "keep looking for an answer, you cannot afford to wait, your heart is strong and that's a good thing, we're controlling this to a degree but something is driving your neural signals and it seems to be outside of my area of expertise. Please keep me posted."
I've had so many ultrasounds and x-rays in the last 12 months that we really haven't had a chance to get on a regular schedule but I suspect that will be the case. My next appt with him is just after the new year. I do have an moderately enlarged left ventricle and a somewhat low ejection fraction.
Before getting sick and during a period of remission I have always been very fit. Lots of long distance cycling, back country skiing, and hiking is probably buying me some time right now.
Again, thank you for the info on Dr. Cheney. Also, Dr. Montoya recognized the pattern immediately and labeled it "cardiovascular instability resulting from autonomic neural issues." In light of all the infectious stuff going on, that seems right on to me.
Hi all,
ust recently been wondering about "low-level" seizure activity that I believ
Very interesting discussion here..I had je Cheney and others have spoken of..
A few of us have been wondering about the possible connection between mild seizure activity and weird, intense perceptual anomalies similar to depersonalization/ derealization (this discussed, oddly, on the Buddhism thread).
Also..does anyone know how in the US you can get a cerebral perfusion scan of any sort covered by insurance?
Dr. Yes,
For myself (and I realize that my experience may not be the same as everyone else), the cardio issues started out mildly and kept on a very steady decline over the course of 3-4 months that left me peering directly into the abyss. Many nights this past summer I took my sleep meds without the least bit of confidence that the meds wouldn't interact with the heart/cerebral vascular/neuro-issues and push me over the edge but I needed sleep. Living like that from April to July definitely put a dent in my old view of reality.
Best to everyone,
Shane
PFO and cerebral perfusion
They are often done when looking for a Patent Foramen Ovale (PFO), a small hole in the hearts atrial septum (see - http://my.clevelandclinic.org/heart/disorders/congenital/pfo.aspx). This hole is actually a fetal feature that allows the blood to by pass the lungs while the fetus is living off of oxygen in the mothers blood. Shortly after birth aflap closes over this hole. It is not uncommon for this closure to be incomplete. Lots of people walk around with a PFO and never know it (I have a small one that is a non-issue - only open a bit upon extreme exertion). In worse case scenarios, these can allow blood to pass directly from the body (viens returning to the heart) to the brain. There are two issues with this. One issue is that the blood is poorly oxygenated. The second issue is that small clots get filtered out in the lungs and when blood bypasses the lungs there is a greater risk of TIAs and strokes.
There are operations to close the hole. Talking with my cardiologist, he has had mixed results. Some people with significant PFOs have great improvement, others have absolutely no improvement. I was also told that when you have the "percutaneous occlusion device" inserted you can feel it with every heart beat and some folks are realy bothered by that.
Shane
Also..does anyone know how in the US you can get a cerebral perfusion scan of any sort covered by insurance?
They are often done when looking for a Patent Foramen Ovale (PFO), a small hole in the hearts atrial septum (see - http://my.clevelandclinic.org/heart/disorders/congenital/pfo.aspx). This hole is actually a fetal feature that allows the blood to by pass the lungs while the fetus is living off of oxygen in the mothers blood. Shortly after birth aflap closes over this hole. It is not uncommon for this closure to be incomplete. Lots of people walk around with a PFO and never know it (I have a small one that is a non-issue - only open a bit upon extreme exertion). In worse case scenarios, these can allow blood to pass directly from the body (viens returning to the heart) to the brain. There are two issues with this. One issue is that the blood is poorly oxygenated. The second issue is that small clots get filtered out in the lungs and when blood bypasses the lungs there is a greater risk of TIAs and strokes.
There are operations to close the hole. Talking with my cardiologist, he has had mixed results. Some people with significant PFOs have great improvement, others have absolutely no improvement. I was also told that when you have the "percutaneous occlusion device" inserted you can feel it with every heart beat and some folks are realy bothered by that.
Shane
Dr. Yes
Shame on You
- Messages
- 868
Thanks Athene, that's really interesting... Koan had mentioned that she had similar symptoms to mine and an EEG during that period showed slight evidence of temporal lobe epilepsy. I had an EEG done this year but it was a standard EEG without the strobe (had I known, I would have asked for the light show!), and was normal. I had a standard brain MRI too, but if I'm not mistaken only a functional MRI can check for hypoperfusion, right?
Shane - Thanks for the info. From what you describe about PFO I know my cardiologist won't order a cerebral perfusion scan for me.. And the neurologist she had referred me to said he could never get insurance to OK it. They were both useless docs, though, so I was hoping...
Shane - Thanks for the info. From what you describe about PFO I know my cardiologist won't order a cerebral perfusion scan for me.. And the neurologist she had referred me to said he could never get insurance to OK it. They were both useless docs, though, so I was hoping...