(I began writing this with the intention of posting it on the oxymatrine thread but it went off on a tangent so I'm posting it here. Sorry it's also a bit long-winded and self-indulgent, however I'd appreciate any feedback.)
I took the supplement, 5-AT yesterday and didn't notice much of anything. I'll experiment with it further in a few days because I took a dose of saphora (oxymatrine herb) and it seems to have induced a bad depression. I was taking this herb along with a few others about six months ago and I suffered several weeks of heavy depression and didn't know why. Perhaps this explains it.
However this cloud may have a silver lining in that it may shed some light on the nature of my PEM. The depression I get with this herb is the same which occurs when I over-exert myself. This was not always a PEM symptom for me but has been the last few years. It's why I can't read for pleasure anymore, and of course kicks in if I've overdone it. Once I've induced the PEM funk there's no delay in further depression; it happens in real time as I exert myself. Even just going for a walk in this state will bring about suicidal thoughts.
The only other treatment to cause this depression/PEM was LDN. It first started when I decided to try a full 50 mg dose of naltrexone. Subsequent to that I haven't been able to tolerate even small doses. But this fits into a sort of theory I've been turning over in my head.
@Hip has pointed out that the depression from saphora/oxymatrine could be the result of interferon activity. I remember reading Cort's write up on Andrew Miller's work and how he saw depression and sickness behavior result from interferon treatment and how it seemed to effect the basal ganglia. His work suggests among other things that this region of the brain and it's reward circuitry may be compromised in some with ME/CFS, and this certainly rings true for me.
http://www.healthrising.org/blog/20...nflammation-fatigue-chronic-fatigue-syndrome/
I've posted elsewhere about how opioids and other drugs that stimulate the reward circuitry block my PEM and reverse many of my bizarre ME/CFS symptoms. I know my reward system is not functioning as it should. I believe this is innate as I've had problems with addiction in the past, but I think it's made far worse by my ME/CFS. So when I fix this glitch with something that produces reward, besides feeling alive for a change, suddenly my immune/ME symptoms resolve. Naltrexone, which blocks the opioid receptors (which factor into reward), makes my condition worse. Interestingly,
@Tristen has also written about his tendency toward addiction and he did very badly on LDN, did so much better on opioids, and now has found considerable relief with suboxone. Suboxone also acts as an opioid agonist. I don't think the similarities between his and my experiences and our addictive history is coincidence. He also speaks of immune markers normalizing with suboxone therapy.
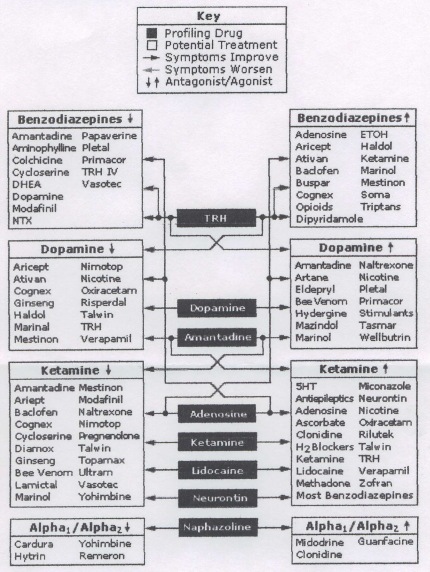
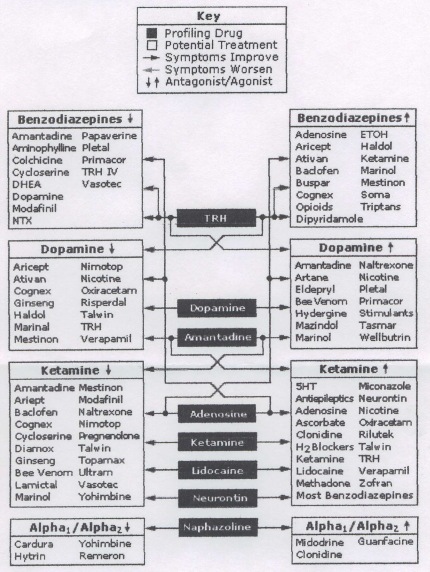
So how do immune symptoms significantly improve with opioids/suboxone? I think the best explanation for this may lie in Jay Goldstein's work. His theory of the disease is that there's dysfunction in the lymbic system and that this causes regulatory issues that lead to the symptoms of ME/CFS, even the strange ones. That's my layman's understanding of it, anyway. And he suggests there are many different pathways that can lead to the dysfunction that he tries to identify and treat with a number of psychotropics. It just so happens that my limbic glitch is best addressed by those in the upper-right hand box of his treatment guide, specifically those that can lead to addiction. So this is but one way in which the lymbic system can become problematic.
Andrew Miller speaks about the issues that may pertain to this basal ganglia condition and make it difficult to treat. One is that not enough dopamine is being produced because of conversion problems arising from oxidative stress. Another is that even with enough dopamine the circuitry does not work properly. This second bit resonates with me as I can tell when my reward system is functioning better based on my creativity playing guitar, and this only happens if my oxidative stress is lowered. For instance methylphenidate will do little but make me anxious and later depressed if I take it while oxidative stress is high, and it actually can block my PEM and normalize various symptoms when oxidative stress is lower. Unfortunately it's effects are unsustainable as receptors lose their sensitivity, and because it has a negative effect on redox/oxidative stress in the long run.
Interestingly Miller posits that an imbalanced ratio of phenylalanine to tyrosine in the blood may be an indication of the problem, as the oxidative stress decreases BH4 and slows conversion of phenylalanine to tyrosine and then tyrosine to dopamine. My phenylalanine has been in the upper 5% and my tyrosine in the lower 10%. However I believe the real problem lies in the oxidative stress compounding the problem in lymbic functioning. Perhaps this is universal in those of us with ME/CFS, as Goldstein suggests, even if through different lymbic pathways.
I figure all this might explain the loop that keeps me ill: oxidative stress leading to an exacerbation of my innate glitch, which then leads to more oxidative stress. Round and round.
Hope this makes some sense to someone...