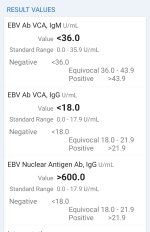
Oh ok, I lost EBV VCA IgG antibodies. Ebna is really high (over 600) so I think I have reactivated EBV. Is your EBV early antigen positive on your latest lab?
I'm currently bedridden atm and unable to get tested for reactivated EBV/CMV/hhv6, etc. May I ask what are the signs and symptoms of reactivated EBV, CMV or hhv6? I'm going to have try to buy generic valtrex or Famvir. I don't think I can buy generic valcyte.
Do you know if Famvir have antiviral activity against CMV/HHV-6? Thanks
I'm in Australia and testing here we don't get a titre level given, it's either positive or negative.
The reactivation symptoms for cmv are typical viral symptoms of lethargy headaches, sore glands and general aches and pains.
My blood work before antivirals and about 7 years after cfs onset, showed total lymphocytes elevated and all my t cell lymphocytes elevated eg cd3, cd4, cd8 etc. The pathology results said lymphocytosis, appears to be a viral infection.
This was done by a new Dr at the time who was familiar with cfs and antivirals. We did the lymphocyte testing again 3 months later in case the first test was just a cold flu type virus. The results were the same and this was when I started antivirals/famvir. It took 3 months before I started to notice things shifting. Blood work showed my total lymphocytes had come down to normal range but my lymphocyte t sub sets were all still elevated. It took 12 months for them to come down where most were within normal range except cd8 T cells which was barely above normal and is commonly seen in ebv and cmv infections.
After this 12 month period I changed to valtrex as it was alot cheaper drug at the time. But over the next 3 month my symptoms returned and my blood worked showed another viral reactivation, ebv or cmv or both as the lymphocyte subset test is non specific. My total lymphocytes and lymphocyte sub sets were all elevated and pathology report said the same thing, lymphocytosis and appears to have a viral infection.
So I started back on famvir and improvement in symptoms and blood work repeated as before.
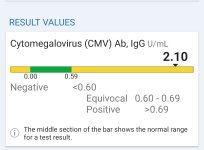
In Australia they don't use igg titre levels or give out titre levels. All they say is a positive igg test just means you've had the infection before. Although I somehow managed to get a cmv titre level test once, which they may do for hiv pts and I must have slipped through the cracks as they refused to do the test again. I can't recall my cmv titre level, only that it was high enough going by Dr Lerners opinion to be classed as reactivated cmv plus at the time I had been on antivirals for a few months when I got this test. Otherwise the only testing available to us to indicate any sort of reactivation is a lymphocyte subset test and it's very non specific to what infection, but for famvir to lower these lymphocyte markers, it's a strong indicator it's probably cmv and maybe ebv.
Also I was involved in a cfs study testing nk function over an 18month period while I was on antivirals. My nk function was very low during this time period I was in the study.
Also 75% of the time I get blood work done, my neutrophils are classed as moderately low.
Also, going off Dr Lerners work valtrex will work for ebv but if you have cmv or hhv6 then it probably won't and that's been my personal experience. Anecdotally some drs have found famvir to work on cmv and hhv6 and is far less toxic and that's my personal experience as well. Dr Lerner used quite high doses which I never approached. My first few years I used famvir at 250mg twice a day and then moved to 500mg twice a day, which I'm currently on.
Antivirals really are a trial and error treatment and it takes time to see results. Atleast 3 months minimum to notice anything and 6-12 months for obvious improvements in general. I wouldn't say they are a cure but they can play a big role in one's improvement. If a person doesn't notice anything after 3 months I'd consider dropping it and look into something else, although sometimes stopping a treatment is needed to tell how much it's helping and if it's worth pursuing.
Good luck



.