Just spit-balling...
In
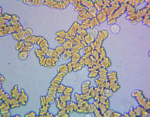
hereditary spherocytosis (HS), red blood cells (RBCs) are unable to maintain their normal form of a biconcave disc. This means they can't deform properly through the smallest capillaries, where they usually fold over, like a taco, and then bounce back.
HS is associated with marked splenomegaly and gallstones. Both features are due to the short RBC lifespan as you note, being broken down in the spleen and releasing their haem products as conjugated bilirubin. I think the short lifespan is due to the damage they sustain squeezing through the small capillaries as larger spherical forms. I don't believe marked splenomegaly and gallstones are common in ME patients.
In ME, the RBCs may be completely normal, and able to deform appropriately. But what if the micro-thrombi circulating with them are sufficient to impede their passage through the smallest capillaries? This would mean the RBCs don't get damaged, but are slow.
Slower RBC transit would mean that more O2 is extracted from each RBC, leading to lower SvO2, as observed by Dr. Khan on his venous blood gas. The tissues are still being starved of O2 overall, as the absolute flux of RBCs is decreased due to their slower transit.
A mild-moderate ME patient might have an amount of micro clot that impaired tissue oxygenation during exertion but not at rest. A more severe patient might have so much micro clot affecting their micro-circulation, that they are compromised even at rest. Fatigue affects the muscles and neuroinflammation and cognitive impairment affect the brain. Multiple symptoms ensue.
Aerobic threshold is then reduced and the mitochondrial biochemical pathways shift to compensate.
Could the slower flow through the (high-capacity) microcirculation cause an effective reduction of blood volume and lead to POTS symptoms?
ETA: This all seems to have been thought about previously and was discussed on
Health Rising back in 2018.