COURSE SUMMARY -
Dr Kharrazian chronic fatigue and pain syndromes course
There wasn’t anything in this course that isn’t discussed somewhere on the PR forum. The course was not specifically focused on ME/CFS and was a 2 day course with a huge amount of information. I put some of the info I thought PR members would be interested in below. If anyone wants more detail on something they see below, just ask.
This course addressed various fatigue syndromes including ME/CFS. More time was spent on non-ME fatigue than on ME/CFS. The diagnostic criteria presented for ME/CFS were the Canadian Consensus Criteria and Dr. K did acknowledge the severity and complexity of the condition, stating that the goal as a practitioner was to help the patient have more good days than bad days. He contrasted this with non-ME fatigue where patients typically recover once the underlying cause of the fatigue has been addressed. I appreciated his review of this paper Review of this this paper
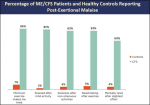
Evidence on Major ME/CFS Symptoms and Manifestations, which contains graphs on the various symptoms of ME/CFS patients compared to healthy controls. Here is an example of one of the graphs:
Dr. Kharrazian identified some of the triggers for ME/CFS discussed on this forum (Viruses and other pathogens, mold, toxins, traumatic brain injury), but he is not an expert in ME/CFS and I was dismayed that he really only advocated testing for EBV stating that you can look indefinitely for the pathogen and not find it. However, in the case studies he presented, he did test for EBV, CMV, HHV6 and Lyme and co-infections.
His treatment suggestions for non-ME fatigue involved identifying underlying mechanisms (thyroid, anemia, glycemic dysregulation, food sensitivities, SIBO, hormonal issues, adrenal concerns, sleep disorders etc). Of course, all of this needs to be addressed in the ME/CFS patient, but the difference is, the ME/CFS is still severely fatigued even after these have been addressed.
His treatment for ME/CFS mostly had to do with addressing the factors that disrupt mitochondrial function and improving mitochondrial function. My opinion was that the approach he outlined makes sense to try, but doesn’t seem to be impactful for many people. Many potential ME/CFS causes were not included and therapies discussed on this forum such as the use of antivirals, high dose thiamine, Oxymatrine, LDN, HBOT, IV saline, blood volume support, useful conventional meds, and many others, were not discussed.
I made two additional posts below:
Post 1- ME/CFS and Pain Syndrome treatment – this would be the most relevant info
Post 2- Everything else – Mitochondrial dysfunction and causes, Differential diagnosis of fatigue, Important testing, mechanisms behind chronic pain