I'm making a second reply to your post because I noticed a few days ago a potential discrepancy in the data being presented in Prof Phair’s graph you attached compared to what is known in the literature with respect to the activity of the IDO2 enzyme.
In the graph(s), which is a Michaelis-Menten presentation with the y-axis labeled as flux instead of rate of reaction (because more than one enzyme is being evaluated), the plot for IDO2 would appear to give a Km value of about 200 micromolar (μM). (Km is the concentration of substrate, in this case tryptophan, with which the enzyme can achieve one-half its maximum reaction rate. The smaller the Km value the greater the affinity the enzyme has for its substrate.)
A Km of 200 μM for IDO2 seems to be much too small (i.e., too good) compared to the three literature values I found:
In a
2011 study, purported to be the first kinetic study of IDO2, a minimum Km was determined of “at least”
4060 μM. (The researchers weren't able to determine an exact value because IDO2 has such a low affinity for tryptophan and because they didn't use a high enough tryptophan concentration in their experiments,)
In a
2014 study a Km value of
6809 μM was found.
And in a
2016 study, a Km value of
9360 μM for IDO2 was found, which is experimentally very comparable to the 2014 value.
So the appearance is that the Km value from Phair's plot is on the order of at least 30 times smaller than one might expect. Although perhaps I've misinterpreted something or there's otherwise some simple explanation for the seeming discrepancy.
But if the above is correct, then IDO2 wouldn't seem to be very relevant in helping to bring down the elevated intracellular tryptophan levels Phair appears to have found in some ME/CFS patients. And indeed the literature is indicating that there is apparently no difference in tryptophan and kynurenine levels in people whether they have a functional IDO2 gene or not.
In fact, the growing consensus, since IDO2 was first discovered in 2007, seems to be that IDO2 is probably not very physiologically important as an enzyme with respect to the catabolism of tryptophan, and that instead its role may actually be non-enzymatic as an immunomodulatory or regulatory gene or protein.
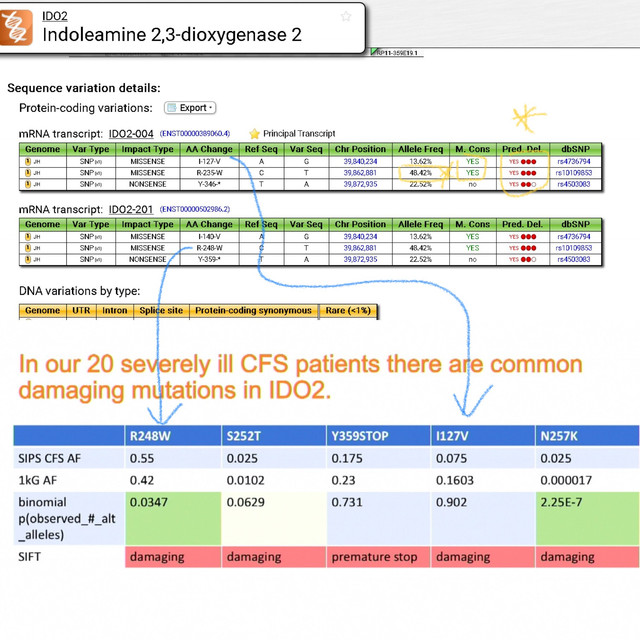
So even though very common in the general population, it might be that a defective IDO2 in ME/CFS patients is somehow a contributor of the elevated tryptophan levels in the first place rather than not providing a way to decrease tryptophan levels that have caused IDO1 to become inhibited.
(Note that it should be relatively easy to at least test whether tryptophan catabolism is really needing to be increased in ME/CFS by using interferon-gamma in Ron Davis's nanoneedle assay in order to upregulate IDO1.)
In any event I very much like and appreciate the line of research that Dr Phair is doing and that the whole Ron Davis/OMF team is doing for that matter.
....