Dx Revision Watch
Suzy Chapman Owner of Dx Revision Watch
- Messages
- 3,061
- Location
- UK
Comment in response to WAMES brief report re recent update on ICD-11:
Twitlonger: http://tl.gd/n_1sr4kdh
Comment in response to WAMES brief report re update on ICD-11:
https://wames.org.uk/cms-english/me-cfs-no-longer-classified-as-bodily-distress-disorder-bdd/
January 27, 2020
Thank you WAMES for highlighting this recent development for ICD-11 and for your kind words. I'd like to take this opportunity to provide a little more context:
In ICD-10, there isn't a category, as such, called "Medically unexplained symptoms (MUS)". But most of the categories in the ICD-10 F45 Somatoform disorders block incorporate the concept of "medically unexplained symptoms".
The IAPT service makes use of the F45 codes as there is no specific ICD-10 code for "MUS".
Most of the ICD-10 Somatoform disorders categories between F45.0 and F45.9 have been replaced for ICD-11 with the new single category, "Bodily distress disorder (BDD)" with Mild; Moderate; and Severe specifiers.
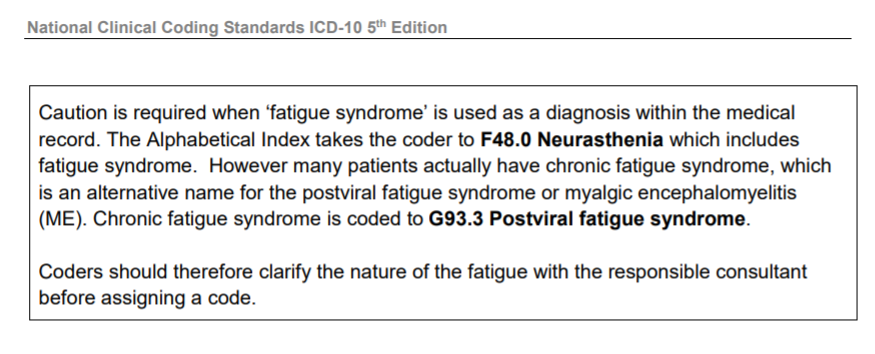
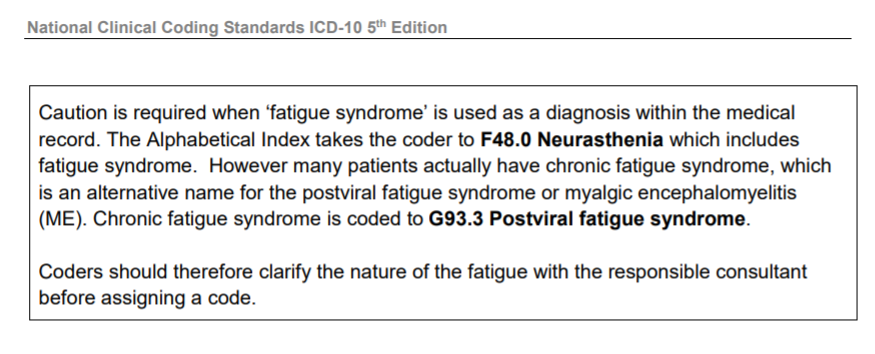
ICD-10's F48.0 Neurasthenia and its inclusion term, Fatigue syndrome, are also subsumed and replaced by this new "Bodily distress disorder (BDD)" category.
ICD-10 has an exclusion for the G93.3 terms under F48.0 Neurasthenia which redirects the coder or clinician to the G93.3 listing.
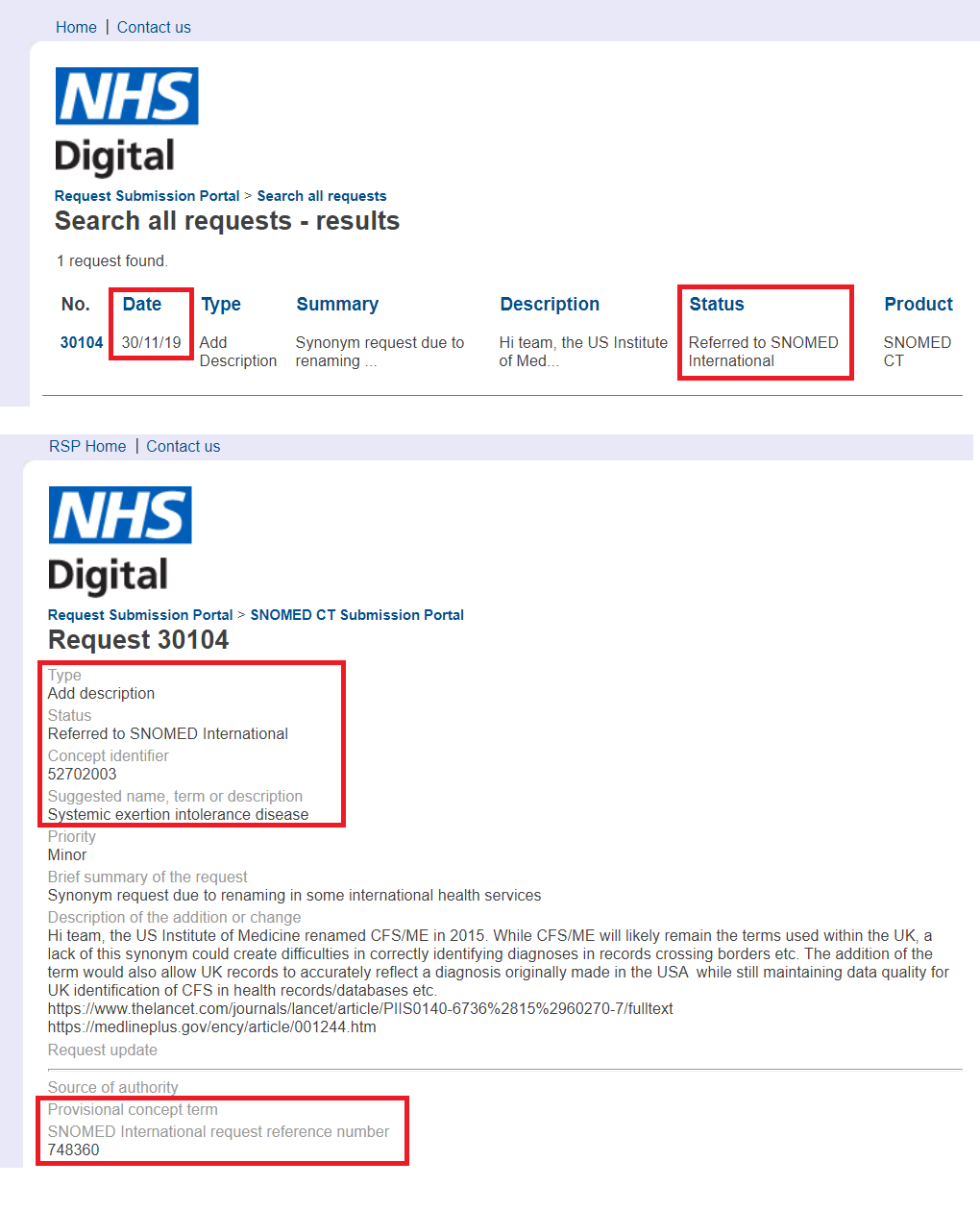
The NHS Digital publication: "National Clinical Coding Standards ICD-10 5th Edition" contains this advisory note for coders and clinicians in relation to F48.0:
https://dxrevisionwatch.files.wordpress.com/2019/04/clinical-standards-5th-edition.png
But this exclusion for the ICD-10 G93.3 terms wasn't carried forward for the draft of ICD-11 and neither was the existing exclusion for the ICD-10 G93.3 terms under R53 Malaise and fatigue - so both these issues needed addressing.
In November 2018, the WHO decided that for ICD-11, the G93.3 legacy terms would be retained in the Diseases of the nervous system chapter as following an extensive review, they had determined that "currently there is no evidence to suggest a better place".
They also rejected a proposal submitted by Dr Tarun Dua, on behalf of the Neurology working group, that CFS and ME should be removed from Diseases of the nervous system and reclassified under the Symptoms, signs chapter, as a child of "Symptoms, signs or clinical findings of the musculoskeletal system".
These decisions were supported by the ICD-11 Medical and Scientific Advisory Committee (MSAC) and the WHO-FIC Classification and Statistics Advisory Committee (CSAC).
So PVFS; (B)ME and CFS remain under the Neurology chapter for ICD-11, with PVFS retained as the "Concept Title". BME and CFS are both specified as Inclusions under 8E49 PVFS and take the 8E49 code.
The new ICD-11 category, "Bodily distress disorder" is very similar to the DSM-5's "Somatic symptom disorder (SSD)".
Both potentially capture patients who might previously have been given a diagnosis of one of the F45 Somatoform disorders. But they can also be applied to some patients with chronic, distressing symptoms associated with a diagnosed general medical disease and condition, and to some of those diagnosed with one or more of the so-called "functional somatic syndromes".
So for BDD, the symptoms can be "medically unexplained" or a general medical disease or condition may be causing or contributing to the symptoms.
For BDD, it is not the nature of the symptoms or their aetiology that is the focus, but whether the patient's response to their chronic, distressing symptoms is perceived as "excessive attention" or "maladaptive"; or in the case of a diagnosed general medical condition, if "the degree of attention is clearly excessive in relation to [the disease's] nature and progression".
It can apply to patients with chronic, multiple symptoms or complaining of a single chronic symptom, like pain or fatigue.
Potentially, patients diagnosed, for example, with cancer, angina, diabetes, MS, ME, CFS, Parkinson disease, rare or difficult to diagnose diseases, especially those that present with multiple symptoms, could attract an additional mental disorder diagnosis of "Bodily distress disorder" - if the clinician considers the patient also meets the "Bodily distress disorder" disorder description. Or they could be at risk of being misdiagnosed with "Bodily distress disorder".
Additionally, the term "Bodily distress disorder" has been used since 2007 interchangeably for the differently conceptualised Fink et al (2007, 2010) "Bodily distress syndrome (BDS)" which is already in use in Denmark and beyond, in both research and clinical settings.
Academics, researchers and clinicians are already confusing and conflating ICD-11's "Bodily distress disorder" with the Fink et al "Bodily distress syndrome (BDS)", under which diagnostic construct, Fink and his colleagues subsume and replace CFS, ME, IBS and Fibromyalgia under a single, unifying "BDS" disorder.
Psychiatrists based in the UK are already authoring chapters in books for international paediatric guidelines recommending that children and young people with a diagnosis of ME, CFS where there is not evidence for a viral onset should be considered for a diagnosis of "Bodily distress disorder".
So it has been crucial to secure exclusions under "Bodily distress disorder" for the PVFS; (B)ME and CFS category terms, as this patient group is one of a number of patient groups that will be particularly vulnerable to misapplication of this new ICD-11 category.
(Exclusions for the 8E49 terms under ICD-11's MG22 Fatigue were also submitted for and secured in 2017 and 2019.)
For a PDF copy of the Rationale submitted in support of my Proposal for addition of exclusions for the 8E49 terms see:
Rationale for Proposal for exclusions under BDD, December 02, 2019:
https://dxrevisionwatch.files.wordpress.com/2020/01/rationale-bdd-exclusions-december-02-2019-1.pdf
For a bite-sized overview of the coding of the 8E49 terms in ICD-11, plus annotated screenshots see:
Post #80 on Phoenix Rising Forum:
Updates on ICD-11 and other classification and terminology systems:
https://forums.phoenixrising.me/thr...terminology-systems.59088/page-4#post-2255295
or see Post #377 on S4ME forum:
Updates on ICD-11 and other classification and terminology systems:
https://www.s4me.info/threads/updat...-terminology-systems.3912/page-19#post-232494
For a more detailed overview of the coding of these terms in ICD-11, see the report that was included in the January 2020 edition of the ME Global Chronicle:
Update on classification of PVFS ME CFS for ICD-11 (v2 updated 25/01/20):
https://dxrevisionwatch.files.wordp...assification-of-pvfs-me-cfs-for-icd-11-v2.pdf
Finally, several additional chapters have been added for ICD-11 and the coding structure and chapter numbering has been re-organized.
For ICD-11, Chapter V Mental and behavioural disorders becomes Chapter 06 Mental, behavioural or neurodevelopmental disorders.
Chapter VI Diseases of the nervous system becomes Chapter 08 Diseases of the nervous system, and between these renumbered chapters, a new chapter called: 07 Sleep-wake disorders has been inserted.
I hope your group members and your wider readership will find this additional context helpful.
Suzy Chapman, Dx Revision Watch
Twitlonger: http://tl.gd/n_1sr4kdh
Comment in response to WAMES brief report re update on ICD-11:
https://wames.org.uk/cms-english/me-cfs-no-longer-classified-as-bodily-distress-disorder-bdd/
January 27, 2020
Thank you WAMES for highlighting this recent development for ICD-11 and for your kind words. I'd like to take this opportunity to provide a little more context:
In ICD-10, there isn't a category, as such, called "Medically unexplained symptoms (MUS)". But most of the categories in the ICD-10 F45 Somatoform disorders block incorporate the concept of "medically unexplained symptoms".
The IAPT service makes use of the F45 codes as there is no specific ICD-10 code for "MUS".
Most of the ICD-10 Somatoform disorders categories between F45.0 and F45.9 have been replaced for ICD-11 with the new single category, "Bodily distress disorder (BDD)" with Mild; Moderate; and Severe specifiers.
ICD-10's F48.0 Neurasthenia and its inclusion term, Fatigue syndrome, are also subsumed and replaced by this new "Bodily distress disorder (BDD)" category.
ICD-10 has an exclusion for the G93.3 terms under F48.0 Neurasthenia which redirects the coder or clinician to the G93.3 listing.
The NHS Digital publication: "National Clinical Coding Standards ICD-10 5th Edition" contains this advisory note for coders and clinicians in relation to F48.0:
https://dxrevisionwatch.files.wordpress.com/2019/04/clinical-standards-5th-edition.png
But this exclusion for the ICD-10 G93.3 terms wasn't carried forward for the draft of ICD-11 and neither was the existing exclusion for the ICD-10 G93.3 terms under R53 Malaise and fatigue - so both these issues needed addressing.
In November 2018, the WHO decided that for ICD-11, the G93.3 legacy terms would be retained in the Diseases of the nervous system chapter as following an extensive review, they had determined that "currently there is no evidence to suggest a better place".
They also rejected a proposal submitted by Dr Tarun Dua, on behalf of the Neurology working group, that CFS and ME should be removed from Diseases of the nervous system and reclassified under the Symptoms, signs chapter, as a child of "Symptoms, signs or clinical findings of the musculoskeletal system".
These decisions were supported by the ICD-11 Medical and Scientific Advisory Committee (MSAC) and the WHO-FIC Classification and Statistics Advisory Committee (CSAC).
So PVFS; (B)ME and CFS remain under the Neurology chapter for ICD-11, with PVFS retained as the "Concept Title". BME and CFS are both specified as Inclusions under 8E49 PVFS and take the 8E49 code.
The new ICD-11 category, "Bodily distress disorder" is very similar to the DSM-5's "Somatic symptom disorder (SSD)".
Both potentially capture patients who might previously have been given a diagnosis of one of the F45 Somatoform disorders. But they can also be applied to some patients with chronic, distressing symptoms associated with a diagnosed general medical disease and condition, and to some of those diagnosed with one or more of the so-called "functional somatic syndromes".
So for BDD, the symptoms can be "medically unexplained" or a general medical disease or condition may be causing or contributing to the symptoms.
For BDD, it is not the nature of the symptoms or their aetiology that is the focus, but whether the patient's response to their chronic, distressing symptoms is perceived as "excessive attention" or "maladaptive"; or in the case of a diagnosed general medical condition, if "the degree of attention is clearly excessive in relation to [the disease's] nature and progression".
It can apply to patients with chronic, multiple symptoms or complaining of a single chronic symptom, like pain or fatigue.
Potentially, patients diagnosed, for example, with cancer, angina, diabetes, MS, ME, CFS, Parkinson disease, rare or difficult to diagnose diseases, especially those that present with multiple symptoms, could attract an additional mental disorder diagnosis of "Bodily distress disorder" - if the clinician considers the patient also meets the "Bodily distress disorder" disorder description. Or they could be at risk of being misdiagnosed with "Bodily distress disorder".
Additionally, the term "Bodily distress disorder" has been used since 2007 interchangeably for the differently conceptualised Fink et al (2007, 2010) "Bodily distress syndrome (BDS)" which is already in use in Denmark and beyond, in both research and clinical settings.
Academics, researchers and clinicians are already confusing and conflating ICD-11's "Bodily distress disorder" with the Fink et al "Bodily distress syndrome (BDS)", under which diagnostic construct, Fink and his colleagues subsume and replace CFS, ME, IBS and Fibromyalgia under a single, unifying "BDS" disorder.
Psychiatrists based in the UK are already authoring chapters in books for international paediatric guidelines recommending that children and young people with a diagnosis of ME, CFS where there is not evidence for a viral onset should be considered for a diagnosis of "Bodily distress disorder".
So it has been crucial to secure exclusions under "Bodily distress disorder" for the PVFS; (B)ME and CFS category terms, as this patient group is one of a number of patient groups that will be particularly vulnerable to misapplication of this new ICD-11 category.
(Exclusions for the 8E49 terms under ICD-11's MG22 Fatigue were also submitted for and secured in 2017 and 2019.)
For a PDF copy of the Rationale submitted in support of my Proposal for addition of exclusions for the 8E49 terms see:
Rationale for Proposal for exclusions under BDD, December 02, 2019:
https://dxrevisionwatch.files.wordpress.com/2020/01/rationale-bdd-exclusions-december-02-2019-1.pdf
For a bite-sized overview of the coding of the 8E49 terms in ICD-11, plus annotated screenshots see:
Post #80 on Phoenix Rising Forum:
Updates on ICD-11 and other classification and terminology systems:
https://forums.phoenixrising.me/thr...terminology-systems.59088/page-4#post-2255295
or see Post #377 on S4ME forum:
Updates on ICD-11 and other classification and terminology systems:
https://www.s4me.info/threads/updat...-terminology-systems.3912/page-19#post-232494
For a more detailed overview of the coding of these terms in ICD-11, see the report that was included in the January 2020 edition of the ME Global Chronicle:
Update on classification of PVFS ME CFS for ICD-11 (v2 updated 25/01/20):
https://dxrevisionwatch.files.wordp...assification-of-pvfs-me-cfs-for-icd-11-v2.pdf
Finally, several additional chapters have been added for ICD-11 and the coding structure and chapter numbering has been re-organized.
For ICD-11, Chapter V Mental and behavioural disorders becomes Chapter 06 Mental, behavioural or neurodevelopmental disorders.
Chapter VI Diseases of the nervous system becomes Chapter 08 Diseases of the nervous system, and between these renumbered chapters, a new chapter called: 07 Sleep-wake disorders has been inserted.
I hope your group members and your wider readership will find this additional context helpful.
Suzy Chapman, Dx Revision Watch
Last edited: