- Messages
- 32
Hi again,
I've finally decided to stop taking valacyclovir (Valtrex) because it was triggering significant neuroinflammatory symptoms. After discussing it with my doctor, we've agreed to start with LDN, and once the inflammation is better controlled, we'll consider reintroducing valacyclovir.
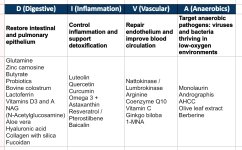
In the meantime, I've been working on simplifying and prioritizing the most relevant supplements for our condition, organizing them by functional areas from most to least critical. I believe that before targeting infections or trying to stimulate the mitochondria—which are in a state of near-hibernation as a survival mechanism—it’s best to begin by restoring epithelial tissues (intestinal and pulmonary), reducing inflammation, and repairing the endothelium.
Here's the summary table—I'd appreciate your feedback on whether you think there's any important supplement missing.
Thanks so much!
D (Digestive)
Restore intestinal and pulmonary epithelium
Glutamine
Zinc carnosine
Butyrate
Probiotics
Bovine colostrum
Lactoferrin
Vitamins D3 and A
NAG (N-Acetylglucosamine)
Aloe vera
Hyaluronic acid
Collagen with silica
Fucoidan
I (Inflammation)
Control inflammation and support detoxification
Luteolin
Quercetin
Curcumin
Omega 3 + Astaxanthin
Resveratrol / Pterostilbene
Baicalin
NAC
PEA (palmitoylethanolamide)
Melatonin
Antihistamines
V (Vascular)
Repair endothelium and improve blood circulation
Nattokinase / Lumbrokinase
Arginine
Coenzyme Q10
Vitamin C
Ginkgo biloba
1-MNA
A (Anaerobics)
Target anaerobic pathogens: viruses and bacteria thriving in low-oxygen environments
Monolaurin
Andrographis
AHCC
Olive leaf extract
Berberine
Lysine
I've finally decided to stop taking valacyclovir (Valtrex) because it was triggering significant neuroinflammatory symptoms. After discussing it with my doctor, we've agreed to start with LDN, and once the inflammation is better controlled, we'll consider reintroducing valacyclovir.
In the meantime, I've been working on simplifying and prioritizing the most relevant supplements for our condition, organizing them by functional areas from most to least critical. I believe that before targeting infections or trying to stimulate the mitochondria—which are in a state of near-hibernation as a survival mechanism—it’s best to begin by restoring epithelial tissues (intestinal and pulmonary), reducing inflammation, and repairing the endothelium.
Here's the summary table—I'd appreciate your feedback on whether you think there's any important supplement missing.
Thanks so much!
D (Digestive)
Restore intestinal and pulmonary epithelium
Glutamine
Zinc carnosine
Butyrate
Probiotics
Bovine colostrum
Lactoferrin
Vitamins D3 and A
NAG (N-Acetylglucosamine)
Aloe vera
Hyaluronic acid
Collagen with silica
Fucoidan
I (Inflammation)
Control inflammation and support detoxification
Luteolin
Quercetin
Curcumin
Omega 3 + Astaxanthin
Resveratrol / Pterostilbene
Baicalin
NAC
PEA (palmitoylethanolamide)
Melatonin
Antihistamines
V (Vascular)
Repair endothelium and improve blood circulation
Nattokinase / Lumbrokinase
Arginine
Coenzyme Q10
Vitamin C
Ginkgo biloba
1-MNA
A (Anaerobics)
Target anaerobic pathogens: viruses and bacteria thriving in low-oxygen environments
Monolaurin
Andrographis
AHCC
Olive leaf extract
Berberine
Lysine
Attachments
Last edited: