here's the official paper:
Radiology: Right Arcuate Fasciculus Abnormality in Chronic Fatigue Syndrome
Abstract
Purpose
To identify whether patients with chronic fatigue syndrome (CFS) have differences in gross brain structure, microscopic structure, or brain perfusion that may explain their symptoms.
Materials and Methods
Fifteen patients with CFS were identified by means of retrospective review with an institutional review board–approved waiver of consent and waiver of authorization. Fourteen age- and sex-matched control subjects provided informed consent in accordance with the institutional review board and HIPAA.
All subjects underwent 3.0-T volumetric T1-weighted magnetic resonance (MR) imaging, with two
diffusion-tensor imaging (DTI) acquisitions and
arterial spin labeling (ASL).
Open source software was used to segment supratentorial gray and white matter and cerebrospinal fluid to compare gray and white matter volumes and cortical thickness. DTI data were processed with automated fiber quantification, which was used to compare piecewise fractional anisotropy (FA) along 20 tracks. For the volumetric analysis, a regression was performed to account for differences in age, handedness, and total intracranial volume, and for the DTI, FA was compared piecewise along tracks by using an unpaired
t test. The open source software segmentation was used to compare cerebral blood flow as measured with ASL.
Results
In the CFS population, FA was increased in the right arcuate fasciculus (
P = .0015), and in right-handers, FA was also increased in the right inferior longitudinal fasciculus (ILF) (
P = .0008). In patients with CFS, right anterior arcuate FA increased with disease severity (
r = 0.649,
P = .026). Bilateral white matter volumes were reduced in CFS (mean ± standard deviation, 467 581 mm3 ± 47 610 for patients vs 504 864 mm3 ± 68 126 for control subjects,
P = .0026), and cortical thickness increased in both right arcuate end points, the middle temporal (
T = 4.25) and precentral (
T = 6.47) gyri, and one right ILF end point, the occipital lobe (
T = 5.36). ASL showed no significant differences.
Conclusion
Bilateral white matter atrophy is present in CFS. No differences in perfusion were noted. Right hemispheric increased FA may reflect degeneration of crossing fibers or strengthening of short-range fibers. Right anterior arcuate FA may serve as a biomarker for CFS.
=====================
I've not read the full text yet but thought it might help to explain a bit about the techniques the researchers used. Basically it's MRI imaging with a couple of extras:
- Arterial spin labelling looks at blood flow but as they found no difference between patients and controls we can ignore that.
- 'Diffusion Tensor Imaging', DTI, is where the action is, and it's used for mapping white matter, the bundles of nerve fibres that connect 'grey matter', which are the brain's main processing centres.
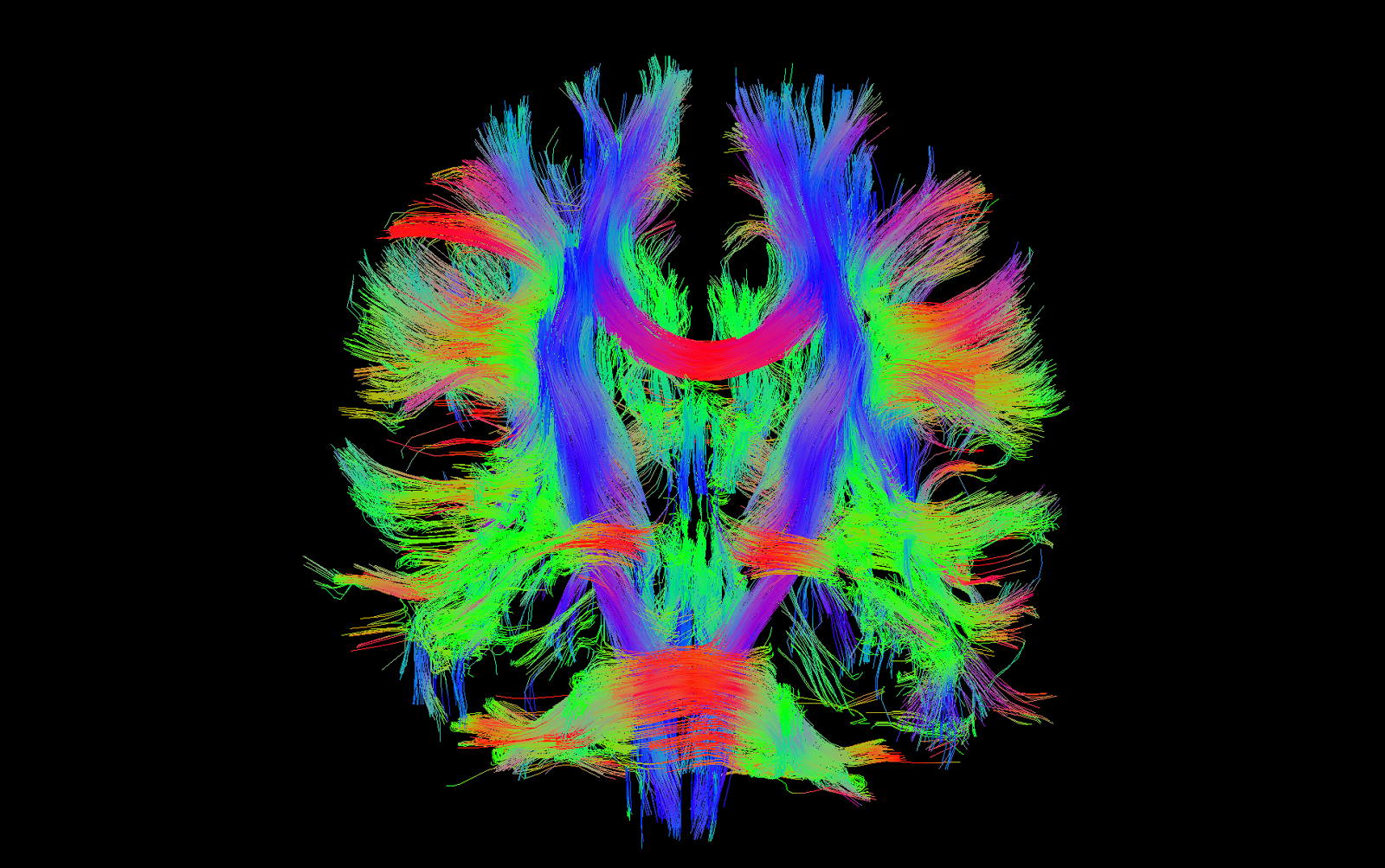
Despite the ugly name, DTI produces some spell-bindingly beautiful images, like
this one, a colour-coded map of nerve tracts in the brain:
From
Wikipedia:
Diffusion Tensor Imaging's main clinical application has been in the study and treatment of
neurological disorders, especially for the management of patients with acute
stroke. Because it can reveal abnormalities in
white matter fiber structure and provide models of brain connectivity, it is rapidly becoming a standard for white matter disorders.
[6]
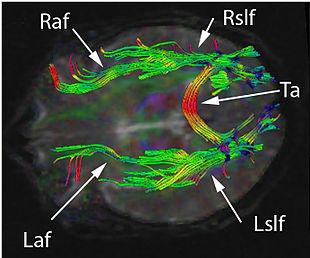
This new study from Stanford found that the nerve tract called the
Arcuate fasciculus showed increased anisotropy in patients compared with controls. What does this mean? Dunno, but the conclusion says: "Right hemispheric increased FA [anisotropy] may reflect degeneration of crossing fibers or strengthening of short-range fibers." Sounds like the authors aren't too sure either.
Here's a pretty picture of the Arcuate fasciculus (R is the right side, L the left side) using the same DTI technology used in this study. Whatever else, this technology is good looking.