I'm putting this out there so hopefully researchers and others can look into this information to verify my claims.
I have looked through 23 23andMe ME/CFS genomes as well as 3 WGS genomes.
There is a common thread. NOD2 mutations seem to have greatly increased prevalence.
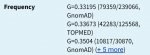
In fact, all 3 WGS samples (100%) have deleterious mutations in NOD2. The first genome has 2 verified pathogenic mutations. The second genome has a single extremely rare predicted damaging variant. And the third genome has two verified pathogenic NOD2 mutations as well as an extremely rare predicted damaging variant (a total of 3 variants). The pathogenic NOD2 mutations were all confirmed with corresponding 23andMe data. And when it comes to 23andMe data, 47.8% of 23 ME/CFS raw data files had a rare and not very common VERIFIED pathogenic mutation. For WGS data specifically, some are predicted by Variant Effect Predictor or Mutation Taster and others are established variants in the NCBI/NIH ClinVar database. 23andMe has some of the important NOD2 variants. But in two WGS samples, there are also predicted NOD2 mutations that are EXTRAORDINARILY rare. The very rare alt allele frequencies were confirmed with gnomAD browser, so they appear to be real variants. The NOD2 mutations range from not very common to rare, but seem to be very common in ME/CFS genomes. And the 23andMe data is self-reported publicly accessible data. So they may be even more common in patients that are verified by ME/CFS expert clinicians. And you need Whole Genome Sequencing to look at the very rare NOD2 damaging variants that I am seeing!
NOD2 is associated with Crohn's Disease, IBD/IBS, and other Autoinflammatory conditions. It's even associated with Fibromyalgia, but no study has been done on NOD2 and it's relationship to ME/CFS. I believe recent GWAS studies completely missed this as well.
NOD2 is important for the recognition and immune response to ssRNA viruses (e.g. Coxsackievirus is an ssRNA virus but herpes viruses are not) and Peptidoglycans (which is a component of the cell wall for almost all bacteria).
I think this is important because what if ME/CFS is an autoinflammatory illness initiated or perpetuated by dysregulation of the NOD-like receptor signaling pathway? What if this could create another negative feedback loop? And most importantly, what if targetted treatments could help ME/CFS symptoms?
Of course, research needs to be done first. This post serves as a call to action for researchers that browse this forum. But to summarize my findings, 100% of ME/CFS Whole Genome Sequence VCF files contained pathogenic and very rare predicted damaging mutations, and 47.8% of 23andMe ME/CFS genomes had pathogenic NOD2 variants that are listed in OMIM.
KEGG NOD-like receptor signaling pathway:
https://www.genome.jp/kegg-bin/show_pathway?ko04621+K10165
I have looked through 23 23andMe ME/CFS genomes as well as 3 WGS genomes.
There is a common thread. NOD2 mutations seem to have greatly increased prevalence.
In fact, all 3 WGS samples (100%) have deleterious mutations in NOD2. The first genome has 2 verified pathogenic mutations. The second genome has a single extremely rare predicted damaging variant. And the third genome has two verified pathogenic NOD2 mutations as well as an extremely rare predicted damaging variant (a total of 3 variants). The pathogenic NOD2 mutations were all confirmed with corresponding 23andMe data. And when it comes to 23andMe data, 47.8% of 23 ME/CFS raw data files had a rare and not very common VERIFIED pathogenic mutation. For WGS data specifically, some are predicted by Variant Effect Predictor or Mutation Taster and others are established variants in the NCBI/NIH ClinVar database. 23andMe has some of the important NOD2 variants. But in two WGS samples, there are also predicted NOD2 mutations that are EXTRAORDINARILY rare. The very rare alt allele frequencies were confirmed with gnomAD browser, so they appear to be real variants. The NOD2 mutations range from not very common to rare, but seem to be very common in ME/CFS genomes. And the 23andMe data is self-reported publicly accessible data. So they may be even more common in patients that are verified by ME/CFS expert clinicians. And you need Whole Genome Sequencing to look at the very rare NOD2 damaging variants that I am seeing!
NOD2 is associated with Crohn's Disease, IBD/IBS, and other Autoinflammatory conditions. It's even associated with Fibromyalgia, but no study has been done on NOD2 and it's relationship to ME/CFS. I believe recent GWAS studies completely missed this as well.
NOD2 is important for the recognition and immune response to ssRNA viruses (e.g. Coxsackievirus is an ssRNA virus but herpes viruses are not) and Peptidoglycans (which is a component of the cell wall for almost all bacteria).
I think this is important because what if ME/CFS is an autoinflammatory illness initiated or perpetuated by dysregulation of the NOD-like receptor signaling pathway? What if this could create another negative feedback loop? And most importantly, what if targetted treatments could help ME/CFS symptoms?
Of course, research needs to be done first. This post serves as a call to action for researchers that browse this forum. But to summarize my findings, 100% of ME/CFS Whole Genome Sequence VCF files contained pathogenic and very rare predicted damaging mutations, and 47.8% of 23andMe ME/CFS genomes had pathogenic NOD2 variants that are listed in OMIM.
KEGG NOD-like receptor signaling pathway:
https://www.genome.jp/kegg-bin/show_pathway?ko04621+K10165
Attachments
Last edited: