Bob
Senior Member
- Messages
- 16,455
- Location
- England (south coast)
Firestormm, my understanding is that Dr Snell's tests are objective biomarkers. He confirmed this as his opinion, in his FDA presentation. Subjective factors, such as effort, motivation and fear etc., do not feature in these tests. So if these results are replicable, then they are very helpful.
I'll explain what I understand about ATWL (aka VTWL), although I'm still learning about it, so I might get some details wrong.
Dr Snell uses a cycle machine, and using CPET (Cardiopulmonary Exercise Testing), he measures the anaerobic threshold for each participant. The anaerobic threshold is the point at which the body starts utilising anaerobic energy production. For athletes, the anaerobic threshold is relatively very high because they are very efficient at producing energy by utilising oxygen. But fitness is fairly irrelevant in this study, because Dr Snell is looking at the differences between first-day thresholds and second-day thresholds, and not the absolute threshold level, and he used sedentary controls.
When the anaerobic threshold is reached, a note is made of the amount of work being carried out on the cycle machine, measured in Watts.
So, it gives you a measure, in Watts, for the point at which each participant reaches their anaerobic threshold.
This is an objective measure, independent of subjective factors such as motivation etc.
If the participant doesn't/can't put in enough effort, then they won't reach the anaerobic threshold, so their results won't be part of the study.
This is really helpful, for various reasons, including that it is an objective biomarker, and because all subjective issues (motivation, pain issues, fear, accusations of laziness etc.) are irrelevant to the results. It objectively demonstrates that CFS patients simply are not as efficient at utilising oxygen, or producing energy, as healthy people. And it also helpfully and objectively demonstrates a post-exertional symptomatic reaction to exercise.
It makes me think of Julia Newton's recent research in which muscle tissue from CFS patients produced 20 times as much (lactic?) acid as healthy controls, when grown in a lab and subjected to simulated exertion via electric shocks. Lactic acid is produced by anaerobic energy production.
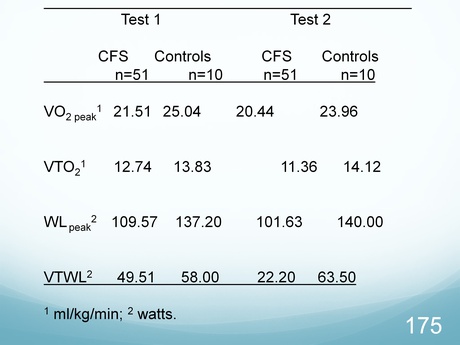
Thinking about post-exertional malaise, notice that, on average, the work-load at anaerobic threshold for healthy controls increased on day two (i.e. their fitness improved), whereas the work-load at anaerobic threshold for CFS patients decreased (dramatically) on day two (i.e. their fitness deteriorated)... See 'VTWL' in graph, below...
I'll explain what I understand about ATWL (aka VTWL), although I'm still learning about it, so I might get some details wrong.
Dr Snell uses a cycle machine, and using CPET (Cardiopulmonary Exercise Testing), he measures the anaerobic threshold for each participant. The anaerobic threshold is the point at which the body starts utilising anaerobic energy production. For athletes, the anaerobic threshold is relatively very high because they are very efficient at producing energy by utilising oxygen. But fitness is fairly irrelevant in this study, because Dr Snell is looking at the differences between first-day thresholds and second-day thresholds, and not the absolute threshold level, and he used sedentary controls.
When the anaerobic threshold is reached, a note is made of the amount of work being carried out on the cycle machine, measured in Watts.
So, it gives you a measure, in Watts, for the point at which each participant reaches their anaerobic threshold.
This is an objective measure, independent of subjective factors such as motivation etc.
If the participant doesn't/can't put in enough effort, then they won't reach the anaerobic threshold, so their results won't be part of the study.
This is really helpful, for various reasons, including that it is an objective biomarker, and because all subjective issues (motivation, pain issues, fear, accusations of laziness etc.) are irrelevant to the results. It objectively demonstrates that CFS patients simply are not as efficient at utilising oxygen, or producing energy, as healthy people. And it also helpfully and objectively demonstrates a post-exertional symptomatic reaction to exercise.
It makes me think of Julia Newton's recent research in which muscle tissue from CFS patients produced 20 times as much (lactic?) acid as healthy controls, when grown in a lab and subjected to simulated exertion via electric shocks. Lactic acid is produced by anaerobic energy production.
Thinking about post-exertional malaise, notice that, on average, the work-load at anaerobic threshold for healthy controls increased on day two (i.e. their fitness improved), whereas the work-load at anaerobic threshold for CFS patients decreased (dramatically) on day two (i.e. their fitness deteriorated)... See 'VTWL' in graph, below...

