Learner1
Senior Member
- Messages
- 6,326
- Location
- Pacific Northwest
Though this news came out about Alzheimer's, I'm wondering if it affects patients with POTS and ME/CFS:
"Discovery of New Role for the Brain’s Immune Cells Could Have Alzheimer’s Implications - Neuroscience News" https://neurosciencenews.com/microglia-blood-brain-19485/
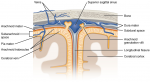
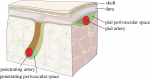
“Precise blood vessel function is critical to accommodate the extreme energy demands of the brain for normal brain function,” said UVA’s Ukpong B. Eyo, PhD, of UVA’s Department of Neuroscience, the UVA Brain Institute and UVA’s Center for Brain Immunology and Glia (BIG). “These findings suggest previously unknown roles for these brain cells in the proper maintenance of blood delivery to the brain and provide novel opportunities to intervene in contexts where blood perfusion to the brain is impaired.”
"Discovery of New Role for the Brain’s Immune Cells Could Have Alzheimer’s Implications - Neuroscience News" https://neurosciencenews.com/microglia-blood-brain-19485/
“Precise blood vessel function is critical to accommodate the extreme energy demands of the brain for normal brain function,” said UVA’s Ukpong B. Eyo, PhD, of UVA’s Department of Neuroscience, the UVA Brain Institute and UVA’s Center for Brain Immunology and Glia (BIG). “These findings suggest previously unknown roles for these brain cells in the proper maintenance of blood delivery to the brain and provide novel opportunities to intervene in contexts where blood perfusion to the brain is impaired.”