percyval577
nucleus caudatus et al
- Messages
- 1,320
- Location
- Ik waak up
@gregh286  But I think you rejoinder is not going to prevail.
But I think you rejoinder is not going to prevail.
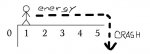
My impression is that delayed PEM is not preceded by an abnormal - this is what we are talking about - feeling related to its trigger. So in your example we felt the first day nicely tired (after being exhausted as well, I guess), and then the second or (possibly strongest) third day we were not getting out of the car - in addition.
But if PEM is delayed than it comes delayed, and there is no preceding PEM, like the normal tiredness in our healthy days. This is how I have understood some reports, there might be others as well possible (i.e. not necessarily required).
I got btw a delayed reaction from mistakes in my then newly discovered diet, and it was exactly 22h later every time, and it lasted for 26-28h. This is what I would like to refind in reports of delayed PEM, and I would think that this bears the sought mechanism inside.
And can muscle aches or repair or breakdown explain the possibility of Pacing? Of course if some special muscles got damaged you might use other ones, and this would be pacing. But is this what we pacing is? I remain sceptical. My impression would be that you walk the one day to the grocer, and the second day you care a bit for your garden. Alot of the same muslces will be involved. But of note may be, I think, that the chain of movements is another one.
In addition it´s my understanding that also mental effort is subject to pacing and PEM. Recently I could play trumpet every three months for some hours. And some years earlier I needed to shift my mental activity - as far as it was possible at all - every four months.
In regard of PEM, where M stands for Malaise, the CCC (point 2) make the additional proposal of something that would be abbreviated PEF, with F for Fatique.
My impression is that delayed PEM is not preceded by an abnormal - this is what we are talking about - feeling related to its trigger. So in your example we felt the first day nicely tired (after being exhausted as well, I guess), and then the second or (possibly strongest) third day we were not getting out of the car - in addition.
But if PEM is delayed than it comes delayed, and there is no preceding PEM, like the normal tiredness in our healthy days. This is how I have understood some reports, there might be others as well possible (i.e. not necessarily required).
I got btw a delayed reaction from mistakes in my then newly discovered diet, and it was exactly 22h later every time, and it lasted for 26-28h. This is what I would like to refind in reports of delayed PEM, and I would think that this bears the sought mechanism inside.
And can muscle aches or repair or breakdown explain the possibility of Pacing? Of course if some special muscles got damaged you might use other ones, and this would be pacing. But is this what we pacing is? I remain sceptical. My impression would be that you walk the one day to the grocer, and the second day you care a bit for your garden. Alot of the same muslces will be involved. But of note may be, I think, that the chain of movements is another one.
In addition it´s my understanding that also mental effort is subject to pacing and PEM. Recently I could play trumpet every three months for some hours. And some years earlier I needed to shift my mental activity - as far as it was possible at all - every four months.
In regard of PEM, where M stands for Malaise, the CCC (point 2) make the additional proposal of something that would be abbreviated PEF, with F for Fatique.
Last edited: