Here are the remaining pages of our proposal and rationale:
Pages 9 to 14
The full Proposal and Rationale can be downloaded here, or there is a PDF attached to Post #137.
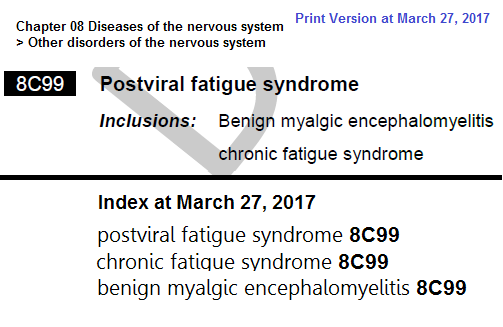
Page 9
Rationale
In July 2015, the authors provided Dr Robert Jakob
(WHO, ICD-11 MMS Joint Task Force) and Ms Anneke Schmider
(ICD-11 Revision Project Manager) with background materials and literature sources on myalgic encephalomyelitis and chronic fatigue syndrome for the consideration of the
Topic Advisory Group for Neurology and to inform the revision process. This section includes selected of those materials plus new materials that have been published since then.
1. Scientific evidence that exists for neurological dsyfunction: The document
Evidence Supporting a Classification of ME and CFS in the Neurological Chapter [1] summarizes many of the neurological and neurocognitive studies in this disease going back to the early 1990s.
PDF: Evidence Supporting a Classification of ME and CFS in the Neurological Chapter 2017
http://bit.ly/2nPj8Vv
In addition to a list of relevant neurological studies, this document includes a 2011 review that summarized evidence of reduction in gray matter volume, reduction in blood flow in the brain, increases in brain lactate levels, changes on MRI and EEG, evidence of autonomic dysfunction, neuroendocrine dysfunction, the presence of abnormal proteins in the spinal fluid, and neurocognitive changes that include deficits in attention, memory and reaction time [2].
This document also includes a 2016 presentation by Professor AnthonyKomaroff, Harvard Medical School, in which he discussed more recent studies that demonstrated brain inflammation that varies with disease severity and also studies showing impaired functional connectivity in the brain [3]. In that presentation, Komaroff concluded with the hypothesis that
"low grade brain inflammation causes the symptoms of ME/CFS and this involves a connection between the brain, the immune system and possibly in some people the gut." He went on to state that according to this hypothesis,
"there are different factors that can trigger ME/CFS but the hypothesis goes they all end up causing low grade inflammation in the brain and that low grade inflammation causes the symptoms of the illness."
Page 10
References:
1 Evidence Supporting a Classification of ME and CFS in the Neurological Chapter 2017.
http://bit.ly/2mwLvYE
2 Komaroff AL, Cho TA. Role of infection and neurologic dysfunction in chronic fatigue syndrome.
Semin Neurol July 2011.
http://dx.doi.org/10.1055/s-0031-1287654
3 Komaroff A. Presentation for U.S. disease organization
Solve ME/CFS Initiative. November 2016.
Minute 14:23, 48:46.
Presentation slides:
http://solvecfs.org/wp-content/uploads/2016/11/SolveME-CFS-Webinar-Dr-Komaroff.pdf
2. Recent federal agency reviews and scientific evidence: The Report of the U.S. Institute of Medicine (IOM), recently renamed, "The National Academy of Medicine," contains one of the most comprehensive literature reviews to date of the biomedical evidence for the disease [1]. The report concluded, as have numerous researchers, that the disease is a
"serious, chronic, complex, and multisystem disease" that causes neurological, cognitive, immunological, autonomic, and energy metabolism impairment.
The Report further noted that the hallmark of the disease is post exertional malaise (PEM), where even very limited physical or mental exertion causes an exacerbation of all symptoms that can last for days, weeks or even months. As a result, the IOM concluded that
"some patients diagnosed by other criteria, such as the Fukuda [CFS] definition, will not fulfill" the IOM's recommended diagnostic criteria. Noting the differences in inclusion and exclusion criteria between CFS and ME definitions, the IOM stated
"a diagnosis of CFS is not equivalent to a diagnosis of ME."
The IOM Report firmly dismissed the idea that this is a psychogenic disease. The Report also noted that the disease can result in prolonged and significant disability with impairment in ability to engage in educational, occupational, social and personal activities; that there is a considerable economic burden associated with these conditions, with many patients unable to continue in employment or in mainstream education; and that 25% of patients are bed- or house-bound during their illness and will require high levels of personal care and assistance from family or social caregivers.
2.1 2014 AHRQ Evidence Review: An evidence review was carried out by the U.S. Department of Health and Human Services' Agency for
Healthcare Research and Quality (AHRQ) in parallel with the IOM evidence review [2]. The 2014 AHRQ review included studies using the Oxford CFS Criteria, studies often based on the biopsychosocial theory that patients' symptoms are caused by fear-avoidant decreased activity and resultant deconditioning.
The AHRQ evidence review on the
Diagnosis and Treatment of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome was published in December 2014 and used as input by the 2015 National Institutes of Health
Pathways to Prevention (P2P) Workshop on Advancing the Research on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome [3].
The 2014 AHRQ review called for the Oxford CFS criteria to be retired because
"it is at high risk of including patients who may have an alternate fatiguing illness, or whose illness resolves spontaneously with time." The NIH P2P report concurred.
In 2016, AHRQ reanalyzed the evidence for Oxford CFS Criteria studies separately from the remaining studies and as a result, issued an addendum that downgraded previous findings once Oxford studies were excluded.
2.2 Highlights of Recent Research: In October 2016, the
International Association for CFS/ME held its biannual conference which highlighted numerous scientific findings. As documented by Professor Anthony Komaroff of Harvard Medical School [4], presentations included studies on brain and nervous system, immunology, the microbiome, epigenetics, energy metabolism and metabolomics. Komaroff summarized that there was robust evidence of an underlying biological process involving a) the brain and autonomic nervous system, b) the immune system, c) energy metabolism, and oxidative and nitrosative stress. Given the scope of biological evidence, he concluded,
"The illness is not simply the expression of physical symptoms by people with a primary psychological disorder."
Page 10
References:
1 National Academy of Medicine. Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness. The National Academies Press; May 2015.
https://www.nap.edu/catalog/19012/b...hronic-fatigue-syndrome-redefining-an-illness
Page 11
2 U.S. Agency for Healthcare Quality and Research. Research Review. Diagnosis and Treatment of Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome. Evidence Report/Technology Assessment Number 219. U.S. Agency for Healthcare Quality and Research. December 9, 2014. Addendum July, 2016. AHRQ Publication No. 15-E001-EF.
https://effectivehealthcare.ahrq.gov/ehc/products/586/2004/chronic-fatigue-report-160728.pdf
3 Green CR, Cowan P, Elk R, O'Neil KM, Rasmussen AL. National Institutes of Health Pathways to Prevention Workshop: Advancing the Research on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome.
Ann Intern Med. 2015.
http://annals.org/aim/article/23228...-advancing-research-myalgic-encephalomyelitis
4 Komaroff A. 12th International IACFS/ME Conference Emerging Science & Clinical Care. October 2016.
http://iacfsme.org/Conferences/2016...6-Summary-Slides/IACFSME-Komaroff-Slides.aspx
3. Options and considerations: As noted above, the IOM expert panel concluded that a comprehensive review of the evidence demonstrates a serious, chronic, systemic disease with dysfunction in neurological, immunological, autonomic and energy metabolism systems.
In SNOMED CT, chronic fatigue syndrome, myalgic encephalomyelitis and other associated terms are already classified under the Parent:
Multisystem disorder.
3.1 Classification of multisystem diseases within ICD-11: Previous editions of ICD have organized diseases into chapters based on aetiology or affected organ or body system. The architecture of ICD-10 does not facilitate scientific and taxonomical representation of diseases with varied manifestations that belong to or affect multiple body systems, for example, systemic lupus erythematosus (SLE) and Behçet disease, or where no single organ system predominates to guide chapter placement.
In 2010, the Revision Steering Group posted a discussion paper on the potential for incorporating within ICD-11 a new chapter for Multisystem diseases [1]. This proposal was subsequently rejected in preference to the consideration of generating a separate linearization from the Foundation, as a "virtual" multisystem chapter [2].
It is currently unclear whether ICD Revision intends to implement a multisystem linearization or whether diseases that would have been candidates for assigning to a "virtual" multisystem chapter will be represented solely through multiple parentage and the explicit listing in the content model of all body systems involved for that entity.
Regardless of how multisystem diseases will be handled in general in ICD-11, it is premature to suggest multiple chapter parentage at this time.
Noting the need for increased biological research, the director of the National Institutes of Health said in a recent article,
"ME/CFS is such a complex condition, affecting so many body systems, that we do not know where the answers will come from." [3].
However, given what we do now know as documented above, the authors see no justification for any proposal for secondary parenting under the
Symptoms, signs or clinical findings, not elsewhere classified chapter or
Mental, behavioural or neurodevelopmental disorders chapter.
References:
1 Aymé, Chalmers, Chute, Jakob (2010). ICD Revision: Discussion paper: Multisystem Disorders.
http://bit.ly/2nnilKW
2 WHO ICD Revision Information Note 19: Multisystem Diseases Chapter in ICD, January 29, 2013.
3 Koroshetz W, Collins F. Moving Toward Answers in ME/CFS. NIH Director's Blog. March 2017.
https://directorsblog.nih.gov/2017/03/21/moving-toward-answers-in-mecfs/
3.2 ICD-11 Joint Task Force position on precedence: General considerations for potential chapter relocations were discussed at a meeting of the Joint Task Force, in July 2016 [1]. According to the meeting Summary Report (
5.2 Key discussion), a general principle was reiterated that:
"...in the absence of compelling evidence mandating a change, legacy should trump with regard to the question of moving certain conditions to new chapters...JTF members confirmed that continuity over time is desirable.
Page 12
Where there is a rationale for change, the changes can be accommodated for, but there was a question about how to justify the effort required to make the changes in data reporting systems in the absence of compelling information indicating that the change makes things better or more accurate."
Although currently a disease of incompletely understood aetiopathogenesis, active research will inform decisions about potential chapter relocation or whether to assign multiple parents. For now, current scientific evidence of neurological impairment and WHO/ICD Revision's position on precedence supports retention of chronic fatigue syndrome and myalgic encephalomyeltis in
Diseases of the nervous system.
References:
1 Fourth Meeting of the JLMMS Task Force, Queensland, Australia, 11-14 July 2016
http://www.who.int/entity/classific....07.11-14_iSummaryMeetingReportQueensland.pdf
3.3 Consideration of creating a sub class under: Other disorders of the nervous system: Until such time that further research supports the creation of, or assignment to a more specific parent class, either within
Diseases of the nervous system, or under another chapter, or assignment to multiple parents, the recommendation is to retain chronic fatigue syndrome and myalgic encephalomyeltis as siblings under
Other disorders of the nervous system.
3.4 Assigning unique codes for chronic fatigue syndrome (CFS) and myalgic encephalomyeltis (ME): In ICD-10, all three terms are coded or indexed to the same code. The IOM Report, the AHRQ Evidence Report, the IACFS/ME Primer for Clinical Practitioners [1] and studies on exercise testing [2] all highlight the importance of post exertional malaise (PEM) as a hallmark symptom, both clinically and in research.
As a result, the IOM specified a clinical criteria that requires PEM, a feature not required for CFS criteria. In addition, researchers internationally are increasingly using the Canadian Consensus Criteria (CCC) [3] or the ME International Consensus Criteria (ME-ICC) [4] - both of which require PEM - to progress research into disease pathology, subtypes, diagnostics, and treatments.
Notably, the IOM Report compared the CFS definitions with the CCC and the ME-ICC and as noted previously, concluded that a CFS diagnosis is not equivalent to an ME diagnosis.
Therefore, the recommendation is to place both chronic fatigue syndrome and myalgic encephalomyeltis in the same location under parent class:
Other disorders of the nervous system, and to assign a unique code to each.
The authors would not support precedence being given to chronic fatigue syndrome as the new concept title, with myalgic encephalomyeltis as the inclusion term, synonym term, or consigned to the Index.
References:
1 ME/CFS: A Primer for Clinical Practitioners 2014.
http://iacfsme.org/portals/0/pdf/Primer_Post_2014_conference.pdf
2 Keller B, Pryor J, Giloteaux, L. Inability of myalgic encephalomyelitis/chronic fatigue syndrome patients to reproduce VO2peak indicates functional impairment.
Journal of Translational Medicine April 2014, 12:104. PMID: 24755065.
http://dx.doi.org/10.1186/1479-5876-12-104
3 Carruthers BM, Jain AK, De Meirleir KL, Peterson DL, Klimas NG, Lerner AM, Bested AC, Flor-Henry P, Joshi P, Powles et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols.
Journal of Chronic Fatigue Syndrome 2003; 11(1): 7-117.
4 Carruthers BM, van de Sande MI, De Meirleir KL, Klimas NG, Broderick G, Mitchell T, Staines D, Powles ACP, Speight N, Vallings R et al. Myalgic Encephalomyelitis: International Consensus Criteria.
Journal of Internal Medicine October 2011; 270(4): 327–338. [PMID: 21777306]
3.5 Consideration of the IOM Report's recommendation for a new case definition and change of nomenclature: The IOM expert panel members were charged with developing clinical diagnostic criteria and making recommendations for a new disease name. The IOM recommended that the term, "chronic fatigue syndrome" should not be used for those patients who meet the IOM's diagnostic criteria and instead, proposed that the term be replaced with
"Systemic Exertion Intolerance Disease (SEID)."
Experts and patients have raised concerns over the suggested new name [1].
Page 13
No proposals have been submitted to the U.S. Coordination and Maintenance Committee to add
"Systemic Exertion Intolerance Disease (SEID)" to the U.S. specific ICD-10-CM. Instead, the CDC has begun to use the hybrid term "ME/CFS" [2] and intends to use that term as it implements the IOM clinical diagnostic criteria. Other agencies within the U.S. Department of Health and Human Services, including the National Institutes of Health, are already using this term and not
"SEID" [3].
Therefore, the authors consider there is currently insufficient evidence or support for incorporating the proposed
"Systemic Exertion Intolerance Disease (SEID)" definition into ICD-11, either as a replacement for one or more of the G93.3 legacy terms or for insertion as an inclusion term, synonym term or index term.
References:
1 Jason LA, Sunnquist M, Brown A, McManimen S, & Furst J. (2015). Reflections on the Institute of Medicine’s systemic exertion intolerance disease.
Polskie Archiwum Medycyny Wewnetrznej. 125(7-8), 576–581. [PMID: 26176405]
2 Unger E, Lin J, Brimmer D, Lapp C, Komaroff A, Nath A, Laird S, Iskander J. CDC Grand Rounds: Chronic Fatigue Syndrome — Advancing Research and Clinical Education.
MMWR Morb Mortal Wkly Rep 2016.
http://dx.doi.org/10.15585/mmwr.mm655051a4
3 A Report from the Federal Partners Meeting of the National Institutes of Health Pathways to Prevention Workshop: Advancing the Research on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). May 2016.
https://prevention.nih.gov/docs/programs/p2p/mecfs-federal-partners-report.pdf
4. Definitions: There are 20 or more CFS and ME definitions, which have been conflated into a single evidence base, with evidence from one definition being assumed to apply to patients meeting any definition [1][2].
Yet, as noted in published research and by U.S. government reports published in 2015-2016, these definitions have significant differences in inclusion and exclusion criteria [2][3][4].
The CFS definitions all require medically unexplained chronic fatigue lasting 6 or more months and either do not require other symptoms or else require one additional or any combination of 4 of 8 common symptoms. As a result, the CFS definitions do not require symptoms recognized by the IOM Report as hallmark symptoms for this disease while allowing the inclusion of primary psychological illness.
The 1991 Oxford definition has most often been used in studies based on a psychogenic disease model. The 1994 Fukuda definition has more often been used for biomedical research. As noted above,U.S. government reports stated that the Oxford CFS definition included patients with other fatiguing illnesses and noted that not all Fukuda CFS patients will meet the IOM’s new clinical diagnostic criteria.
The ME definitions (the 2003 Canadian Consensus Criteria (CCC) uses the hybrid term ME/CFS) and the 2011 ME International Consensus Criteria (ME-ICC) both require hallmark symptoms of the disease such as PEM, sleep dysfunction and neurological/cognitive manifestations and also highlight immunological impairment [3].
Expert clinicians use the CCC in clinical practice; researchers have increasingly used the CCC or the ME-ICC in published research, and the U.S. National Institutes of Health is using the CCC in its current intramural study.
The Institute of Medicine (now the "The National Academy of Medicine") has published new clinical diagnostic criteria, which are based on the Canadian Consensus Review and also require hallmark symptoms such as PEM. The IOM clinical diagnostic criteria have not been officially implemented in U.S. clinical practice and are not in use in other countries.
At this time, there is no single CFS or ME definition that is used worldwide. However, it is possible to describe the core features specified in the CFS and ME definitions.
Definitions
CFS and ME have been historically treated as synonymous but the case definitions encompass different populations.
CFS Definition Features: According to commonly used CFS definitions, CFS is medically unexplained chronic fatigue that is disabling and lasts six months or more for adults, (3-4 months for pediatric). No other symptoms are specifically required, although some CFS definitions do require an optional combination of other common symptoms. CFS is most often described as fatigue that does not get better with bedrest.
ME Definition Features: According to commonly used ME definitions, ME is a
serious, chronic, complex, and multisystem disease that causes neurological, cognitive, immunological, autonomic, and energy metabolism impairment. It is characterized by the hallmark post-exertional malaise in which even small amounts of physical and mental exertion causes an often-delayed exacerbation of all symptoms that can last for days, weeks or even months. Onset can follow an infectious trigger, which is often but not always viral
.
References:
1 Brurberg K, Fønhus A, Larun L, Flottorp S, Malterud K. Case definitions for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): a systematic review.
BMJ Open. February 7, 2014; 4(2): e003973.
http://dx.doi.org/10.1136/bmjopen-2013-003973
2 Jason LA, So S, Evans M, Brown A, Sunnquist M, Im Y, Schafer C. An overview of operationalizing criteria for ME, ME/CFS, and CFS case definitions.
Prev Interv Community. 2015;43(1):1-4. [PMID: 25584523]
3 National Academy of Medicine. Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness. The National Academies Press; May 2015.
https://www.nap.edu/catalog/19012/beyond-myalgic- encephalomyelitischronic-fatigue-syndrome-redefining-an-illness
4 U.S. Agency for Healthcare Quality and Research. Research Review. Diagnosis and Treatment of Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome. Evidence Report/Technology Assessment Number 219. U.S. Agency for Healthcare Quality and Research. December 9, 2014. Addendum July, 2016. AHRQ Publication No. 15-E001-EF.
https://effectivehealthcare.ahrq.gov/ehc/products/586/2004/chronic-fatigue-report-160728.pdf
5 Overview of more commonly used myalgic encephalomyelitis and chronic fatigue syndrome definitions.
http://bit.ly/2niiKfu
[Ends]
[List of 45 links for aggregated references]
[Rationale field]
The Rationale for this Proposal has been appended to the Detailed Explanation for improved accessibility for a stakeholder patient group, some of whom may experience cognitive impairment and visual problems when viewing unformatted plain text manuscripts on computer screens.
A copy of this Proposal and Rationale can be accessed here in PDF format: http://bit.ly/2nLdvHy
[Ends]