sb4
Senior Member
- Messages
- 1,660
- Location
- United Kingdom
I am interested an idea dejurgen posted about on health rising. It is tied to a study which found O2 wasn't being released from blood as much as it should. I asked him to explain how this accounts for carbs intolerance. He gave an interesting explanation which made me think that PDH might not be a problem. So with that in mind I think glucose intolerance due to dejurgens low O2 theory goes something like this.
Cells have low O2, this means they have low energy production. If they are forced to produce more energy they struggle and lactic acid is produced in increasing amounts, this all leads to negative symptoms. When you eat a carb containing meal, those carbs have to be dealt with to prevent BG going to high, so they are shoved into cells however these cells have low O2 so cannot deal with them correctly so lactic acid is produced, etc and symptoms are increased. This doesn't happen with fats as they can easily be dealt with by putting them into fat cells.
So I figure that if I supplied enough glucose for a significant period of time (via low GI foods) to inhibit lipolysis yet not so much that glucose is actively pushed into cells to be dealt with, I could see whether errors in glucose metabolism are the issue in me or whether. Getting those levels right would be very tricky though. I would need to have a small blood glucose peak followed by a slow lowering to baseline. I would need to provide the same level of calories as are utilized during fasting such that the cell isn't forced to use more calories than it was before.
"In other terms, in a rested state, an average person consumes about 3.5 ml of O2 per kilogram body weight per minute or expends about 1 kcal* per kg body weight per hour. This rate of energy expenditure is expressed as 1 metabolic equivalent (MET) (4). Using these common values, it can be calculated that a resting 70 kg man expends around 1680 kcal per day."
If those numbers are correct then I would be consuming about 90kcal per hour in a fasted state. So I need to eat enough low GI starch that would provide roughly this amount per hour in a long drawn out fashon. This is 22g Carbs per hour.
This suggests that fasting RER 0.77-0.78. If I have got this correct, 1 is complete glucose oxidation, 0.7 if fat. So this means that 1/4 of kcals consumed in a fasting state are glucose and 3/4 fatty acids. Fasting BG is around 5 mmol/L and 5L of blood = 25mmol. I can't seem to find anything stating how quickly it is utilized so I will work it out, although this could have already gone wrong in many places. 90kcal * 0.25 glucose = 22kcal glucose used per hour. Glucose 180 g/mol * 0.025 mol = 4.5g of glucose in blood at any moment or 18kcals.
So we use up just over the total amount of glucose in our blood in 1hr. That's pretty convenient. So if I where to replace my fasting calories used from fat with glucose my BG would be 20 mmol/L which is full on diabetes. So if someone has a RER of 1 meaning they are fully oxidizing glucose, why don't they have 20 mmol/L BG? Perhaps in this case glucose is taken out of the blood (and put in) at an enhanced rate to compensate for lack of blood FFA. If this is the case it will be difficult to use BG readings to track how much glucose my tissues are using. Using this logic would it be possible to have a RER of 1 with BG of 5mmol/L?
So I guess if I consumed 20g of low GI carbs per hour I would have some spikes in BG every 30 mins but wouldn't be pushing my cells too my over normal fasting metabolism. If I did this over the course of 6hrs that is 120g carbs total. If I ate this in one meal I would definitely notice an effect however spread out over 6 hrs the effect would be much reduced so I do not think this is a good test of the idea. I would need a steady glucose infusion to provide 90kcals per hour.
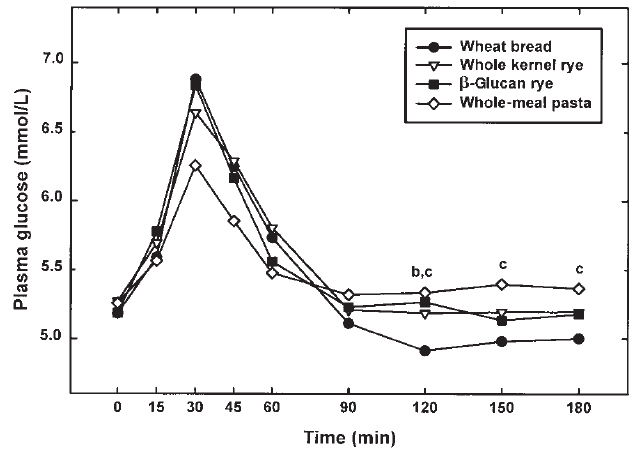
This is after 50g of carbs for each source. A slice of brown bread is around 15g. So if I where to attempt this I could do one slice per hr for 6hrs. My gastroparesis is also a factor which makes this idea kind of bust. I will still post the thread anyway in case I decide to try something similar.
Cells have low O2, this means they have low energy production. If they are forced to produce more energy they struggle and lactic acid is produced in increasing amounts, this all leads to negative symptoms. When you eat a carb containing meal, those carbs have to be dealt with to prevent BG going to high, so they are shoved into cells however these cells have low O2 so cannot deal with them correctly so lactic acid is produced, etc and symptoms are increased. This doesn't happen with fats as they can easily be dealt with by putting them into fat cells.
So I figure that if I supplied enough glucose for a significant period of time (via low GI foods) to inhibit lipolysis yet not so much that glucose is actively pushed into cells to be dealt with, I could see whether errors in glucose metabolism are the issue in me or whether. Getting those levels right would be very tricky though. I would need to have a small blood glucose peak followed by a slow lowering to baseline. I would need to provide the same level of calories as are utilized during fasting such that the cell isn't forced to use more calories than it was before.
"In other terms, in a rested state, an average person consumes about 3.5 ml of O2 per kilogram body weight per minute or expends about 1 kcal* per kg body weight per hour. This rate of energy expenditure is expressed as 1 metabolic equivalent (MET) (4). Using these common values, it can be calculated that a resting 70 kg man expends around 1680 kcal per day."
If those numbers are correct then I would be consuming about 90kcal per hour in a fasted state. So I need to eat enough low GI starch that would provide roughly this amount per hour in a long drawn out fashon. This is 22g Carbs per hour.
This suggests that fasting RER 0.77-0.78. If I have got this correct, 1 is complete glucose oxidation, 0.7 if fat. So this means that 1/4 of kcals consumed in a fasting state are glucose and 3/4 fatty acids. Fasting BG is around 5 mmol/L and 5L of blood = 25mmol. I can't seem to find anything stating how quickly it is utilized so I will work it out, although this could have already gone wrong in many places. 90kcal * 0.25 glucose = 22kcal glucose used per hour. Glucose 180 g/mol * 0.025 mol = 4.5g of glucose in blood at any moment or 18kcals.
So we use up just over the total amount of glucose in our blood in 1hr. That's pretty convenient. So if I where to replace my fasting calories used from fat with glucose my BG would be 20 mmol/L which is full on diabetes. So if someone has a RER of 1 meaning they are fully oxidizing glucose, why don't they have 20 mmol/L BG? Perhaps in this case glucose is taken out of the blood (and put in) at an enhanced rate to compensate for lack of blood FFA. If this is the case it will be difficult to use BG readings to track how much glucose my tissues are using. Using this logic would it be possible to have a RER of 1 with BG of 5mmol/L?
So I guess if I consumed 20g of low GI carbs per hour I would have some spikes in BG every 30 mins but wouldn't be pushing my cells too my over normal fasting metabolism. If I did this over the course of 6hrs that is 120g carbs total. If I ate this in one meal I would definitely notice an effect however spread out over 6 hrs the effect would be much reduced so I do not think this is a good test of the idea. I would need a steady glucose infusion to provide 90kcals per hour.
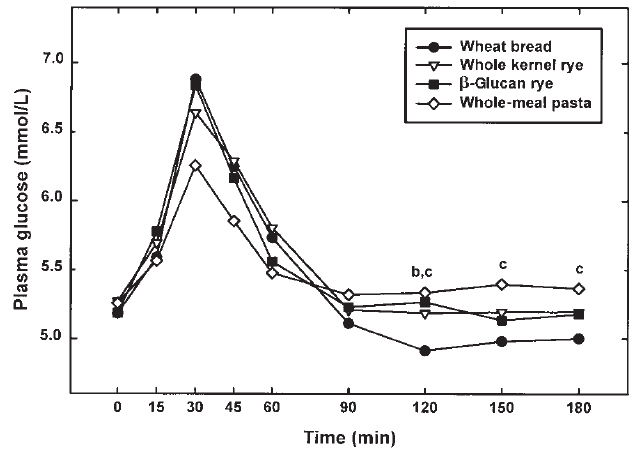
This is after 50g of carbs for each source. A slice of brown bread is around 15g. So if I where to attempt this I could do one slice per hr for 6hrs. My gastroparesis is also a factor which makes this idea kind of bust. I will still post the thread anyway in case I decide to try something similar.
