Simon
Senior Member
- Messages
- 3,789
- Location
- Monmouth, UK
Examining case definition criteria for chronic fatigue syndrome and myalgic encephalomyelitis
Background: Considerable controversy has transpired regarding the core features of myalgic encephalomyelitis (ME) and chronic fatigue syndrome (CFS). Current case definitions differ in the number and types of symptoms required. This ambiguity impedes the search for biological markers and effective treatments.
Purpose: This study sought to empirically operationalize symptom criteria and identify which symptoms best characterize the illness.
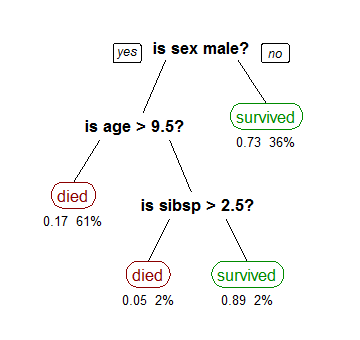
Methods: Patients (n = 236) and controls (n = 86) completed the DePaul Symptom Questionnaire, rating the frequency and severity of 54 symptoms. Responses were compared to determine the threshold of frequency/severity ratings that best distinguished patients from controls. A Classification and Regression Tree (CART) algorithm was used to identify the combination of symptoms that most accurately classified patients and controls.
Results:
A third of controls met the symptom criteria of a common CFS case definition when just symptom presence was required; however, when frequency/severity requirements were raised, only 5% met the criteria.
Employing these higher frequency/severity requirements, the CART algorithm identified three symptoms that accurately classified 95.4% of participants as patient or control: fatigue/extreme tiredness, inability to focus on multiple things simultaneously, and experiencing a dead/heavy feeling after starting to exercise.
Conclusions:
Minimum frequency/severity thresholds should be specified in symptom criteria to reduce the likelihood of misclassification.
Future research should continue to seek empirical support of the core symptoms of ME and CFS to further progress the search for biological markers and treatments.
----
The basic finding that symptom frequency and severity are important in separating patients and controls is interesting. In the PACE recovery paper, the authors argued that most of the population had several mecfs symptoms at any time and implied that patients shouldn't get too hung up on such things - though the population study PACE cited was flawed and in any case showed the symptoms only affected daily activity for a small minority of the healthy.
Background: Considerable controversy has transpired regarding the core features of myalgic encephalomyelitis (ME) and chronic fatigue syndrome (CFS). Current case definitions differ in the number and types of symptoms required. This ambiguity impedes the search for biological markers and effective treatments.
Purpose: This study sought to empirically operationalize symptom criteria and identify which symptoms best characterize the illness.
Methods: Patients (n = 236) and controls (n = 86) completed the DePaul Symptom Questionnaire, rating the frequency and severity of 54 symptoms. Responses were compared to determine the threshold of frequency/severity ratings that best distinguished patients from controls. A Classification and Regression Tree (CART) algorithm was used to identify the combination of symptoms that most accurately classified patients and controls.
Results:
A third of controls met the symptom criteria of a common CFS case definition when just symptom presence was required; however, when frequency/severity requirements were raised, only 5% met the criteria.
Employing these higher frequency/severity requirements, the CART algorithm identified three symptoms that accurately classified 95.4% of participants as patient or control: fatigue/extreme tiredness, inability to focus on multiple things simultaneously, and experiencing a dead/heavy feeling after starting to exercise.
Conclusions:
Minimum frequency/severity thresholds should be specified in symptom criteria to reduce the likelihood of misclassification.
Future research should continue to seek empirical support of the core symptoms of ME and CFS to further progress the search for biological markers and treatments.
----
The basic finding that symptom frequency and severity are important in separating patients and controls is interesting. In the PACE recovery paper, the authors argued that most of the population had several mecfs symptoms at any time and implied that patients shouldn't get too hung up on such things - though the population study PACE cited was flawed and in any case showed the symptoms only affected daily activity for a small minority of the healthy.
Last edited: