View the Post on the Blog
The WHO ICD featured recently in an online article (since withdrawn), which heightened patient concern over what might happen when the current ICD-10 is finally revised. N.A.Wright provides a timely summary of this international classification system, considers some of the issues surrounding the existing and proposed listing, and calls on our advocacy organisations to get involved...
The World Health Organization (WHO) is responsible for producing an International Classification of Diseases – the ICD.
An important document in standardising epidemiological data, the ICD has often been a source of confusion in discussions about ME/CFS.
The ICD is subject to continuous review with updates published annually and major revisions are intended to be produced every ten years. The date for publication of the ongoing full revision has recently been announced as 2017, providing a three year extension to the formal revision process that began in 2007.
Understanding what the ICD is, what its limitations are and how best to engage with the revision process should be a significant focus for ME/CFS advocacy.
The ICD through an ME/CFS Lens
Many ME/CFS patients first gained awareness of the World Health Organization International Classification of Diseases in the various online discussions that surrounded the UK PACE trial and the arguments made against PACE and its associated projects.
As part of the challenge to the PACE research a patient advocacy position was advanced which relied on the classification of ME as a neurological condition under the World Health Organization’s “International Classification of Diseases” (ICD).
This advocacy position can be summed up as, “ME is neurological because the World Health Organization says so”. Unfortunately, it is a position that is poorly founded because the ICD simply does not confer the authority that is implied.
Equally unfortunate is that the WHO itself perhaps overstates its own case by claiming on its website that, “The International Classification of Diseases (ICD) is the standard diagnostic tool for epidemiology, health management and clinical purposes.”
The ICD has very limited clinical application or diagnostic power, and with the exception of Mental Health (see 'Limitations of the ICD' below), has no significant diagnostic role in the health delivery systems of most developed countries.
A far more accurate statement of what the ICD is and what it can be used for, is to be found on the NHS Connecting for Health website:
“ICD-10 is a statistical tool that requires adherence to and application of specified definitions and rules to enable accurate, consistent and comprehensive capture of data for secondary purposes which is undertaken by health informatics professionals – clinical coders.”
A Brief History of International Disease Classification
International disease classification began a century before the United Nations (UN) and WHO came into existence. Building on the work of the British Registrar General from 1837, the first international listings of causes of mortality were accepted by the International Statistical Congress in 1855 and it is from this that the ICD revision numbers commence, the current publication is ICD-10.
By 1900 mortality statistics were augmented with a classification of morbidity by disease and further revisions saw, with the inception of the UN, the adoption by WHO of ICD-6, in 1946. Subsequent revisions were envisaged to take place every 10 years, although slippage at various stages leaves the current published revision at ICD-10 .
ICD-10 is currently under revision and will be replaced by ICD-11, which is scheduled for World Health Assembly approval in May 2017.
The term Benign Myalgic Encephalomyelitis was first included in ICD-8 which was published in 1969 where it was categorised under the heading “Disorders of the Nervous System” with the coding number G93.3. This classification was repeated in ICD-9 (published in 1975) and in ICD-10 (published in 1992).
The replacement for ICD-10 is long overdue and it must be expected that after more than 20 years, as part of the general updating process, some reconsideration of the classification of ME may take place.
Limitations of the ICD
Although vastly more sophisticated than envisaged by the pioneers of international disease statistics, the ICD is still primarily only a system of categorisation which to date has not been a reference of internationally agreed diagnostic criteria.
This may to some extent change with ICD-11 where the inclusion of diagnostic criteria may appear as part of the disease descriptors. There is one part of the ICD which has long standing acceptance as having diagnostic authority, that is Chapter 5: Mental and Behavioural Disorders, which is published in two separate editions, the Blue Book: Clinical Descriptions and Diagnostic Guidelines and the Green Book: Diagnostic Criteria for Research.
The ICD can be compared to the Dewy Decimal System (DDS) which is used throughout the world to give structure to libraries. Just because a book is allocated a given DDS number does not mean that the book lacks characteristics which may see it placed in another category, or that at some future date the category to which that particular book may have been assigned, may have its description changed or be further subdivided.
The book will not change but its system number and place on the shelf might.
The direct comparison between the ICD and the DDS is limited because diseases are not single edition books; research and developments in treatment mean that ‘diseases’ are subject to constant updates and even to full re-writes as well as the production of multiple volumes which may cross categories.
So, unlike a library, not only are the categories within the ICD subject to change, but so also is the material that is contained within the categories. This is why in addition to annual internal updating via the WHO-FIC Committees, there is a notional ten year process of open review; it is understood that for the ICD to remain relevant it must be constantly globally updated.
The fact that ICD-11 is already 12 years late is no doubt evidence of the huge task that this updating represents in the face of unprecedented world wide investment in health research.
In summary, what this means for ME/CFS advocacy is that categorisation within the system has not conferred diagnostic authority and the location of a disease in a particular category only defined what was seen as useful from the perspective of gathering data, at a particular time.
ICD categorisation will always be subject to change, using the ICD as though it were a fixed and authoritatively determined diagnostic statement, rather than a serviceable means of data recording, may not be advisable from an advocacy perspective.
ICD Clinical Modifications
International Classification of Diseases-Clinical Modifications (ICD-CM), are nationally specific adaptations of the ICD categorisation system which may include diagnostic and clinical detail, such that an ICD-CM can be used as a diagnostic and clinical reference within a specific nation’s health provision. ICD-CMs should not be confused with the ICD.
At least 12 countries including the US, Canada, Australia and Germany, employ ICD Clinical Modifications, which serve a variety of purposes in different countries. The US, for example, has a sophisticated process overseen by the Centers for Medicare and Medicaid Services.
Clinical Modifications, although based strictly upon the ICD categorisation, unlike the ICD itself, do have direct clinical relevance for health provision in each relevant country. Though it is important to be clear that updates to the ICD, may not feed directly into the national ICD-CMs.
Each national ICD-CM is subject to national review which may substantially lag behind changes to the ICD. The US in particular trails behind much of the rest of the world by still using a Clinical Modification based on ICD-9, a version long since retired by WHO. ICD-9-CM does have an annual process for updates, but the US doesn’t plan to shift from ICD-9-CM to ICD-10-CM until late 2014.
International Classification of Diseases 11th Revision
The International Classification of Diseases (ICD) 11th Revision is a currently active process, and it is this process that will produce the documents which will be collectively known, once approved by the World Health Assembly, as ICD-11.
According to the WHO:
“ICD-11, is now being prepared. The development phase will continue for three years and ICD-11 will be finalized in 2017. For the first time, through advances in information technology, public health users, stakeholders and others interested can provide input to the beta version of ICD-11 using an online revision process. Peer-reviewed comments and input will be added through the revision period. When finalized, ICD-11 will be ready to use with electronic health records and information systems. WHO encourages broad participation in the 11th revision so that the final classification meets the needs of health information users and is more comprehensive.”
Participation is additionally invited and public health users, clinicians, researchers and other stakeholders can register to provide input into the drafting process and to assist in support activities, such as participation in field tests and translations.
Access and the registration portal is here: ICD-11 Beta Draft (or click the image above).
While open to individuals, achieving effective influence will almost certainly need the force of established organisations supported by acknowledged medical expertise. Co-ordinated action by a coalition of such organisations would be the ideal.
ME/CFS and ICD-11
Because they affect diagnosis and treatment provision directly, the various national ICD Clinical Modifications have the most immediate impact upon patients. Nevertheless the positioning of ME/CFS within the ICD system as a whole is important because such an international reference can influence the context in which the illness is considered in terms of research and health service resource allocations, across the globe.
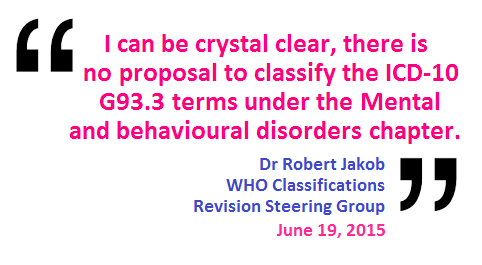
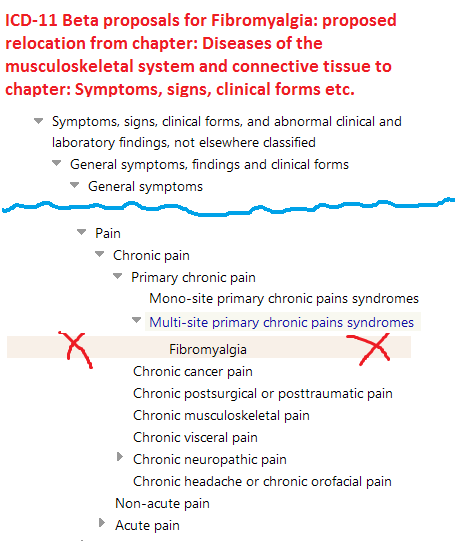
Changes to the structure and chapter organisation between ICD-10 and ICD-11 will mean that many ICD terms will be presented differently. A new code numbering system applies across the entire classification, so the current coding position of G93.3 for Benign Myalgic Encephalomyelitis, is likely to change, though categories with ICD-10 equivalent terms will be cross referenced to the current ICD-10 codes. Some parent class terms are being retired and there are also proposals for changes to category hierarchies.
In early 2013 the proposal displaying in the Beta drafting platform was to make CFS the ICD Title code, with Benign Myalgic Encephalomyelitis specified as the Inclusion Term to CFS; and PVFS listed under Synonyms to CFS. There will be significantly more textual content across all chapters of ICD-11 and all ICD Title codes will be allocated Definitions and selected other "Content Model" descriptors.
Patient advocacy groups need to monitor these developments and to seek to influence, not just the working proposals on chapter location and hierarchy, but to also ensure that proposals for definitions and other textual content reflect the long term interests of patients.
Dx Revision Watch makes the following interesting observation:
“Unlike ICD-10, multiple parents are allowable under ICD-11: TAG Neurology may intend to assign one or more of these terms to multiple parents within the same chapter, or to code to parents located under more than one chapter, for example, under parent classes, Symptoms, signs and clinical findings involving the nervous and musculoskeletal system or Functional disorders of the nervous system (located under both Chapter 07 and Chapter 19), ...”
It would certainly be a pragmatic approach to have ME/CFS under multiple listings. While epidemiological data collection would be somewhat complicated, multiple listings would allow the accommodation of future nomenclature changes relative to developments in research and treatment.
Future Work
Through her website, Dx Revision Watch, Suzy Chapman has been monitoring and reporting on the progress of the revision to PVFS (Post Viral Fatigue Syndrome), BME (Benign Myalgic Encephalomyelitis) and CFS (Chronic Fatigue Syndrome) for ICD-11 for the last five years. Suzy has also monitored and reported on the revision of the ICD-10 and DSM (Diagnostic and Statistical Manual of Mental Disorders) Somatoform disorders.
However, Suzy has recently announced that for personal and political reasons she is stepping back from the work she does via her site. She does not anticipate publishing and circulating new content, although there will be some updates to existing reports.
The WHO is an international body: our reliance on a single volunteer in a single country to monitor and report on the ICD process for the global ME/CFS patient and professional population, has been neither fair, nor reasonable.
Suzy Chapman's stepping back should be seen as a wake-up call to patient and advocacy organisations to get involved.
ICD-11 need not be seen as inherently a threat to the interests of ME/CFS patients; however to make the most of the opportunities that the ICD-11 process offers, patient organisations must become active participants in the development of the ICD-11 draft over the next three years.
The first objective of that participation should be to ensure that the lack of transparency that currently affects the ICD-11 position on ME/CFS, (and to which patients have been alerted by Dx Revision Watch, see: A Beta draft black hole), is urgently resolved.
*note ME/CFS is used in this article as a generic term, it doesn’t imply any diagnostic preference.
**The author thanks Suzy Chapman for helpful comments and suggestions in relation to the ICD-11 revision process. All views expressed are the author’s own.
Phoenix Rising is a registered 501 c.(3) non profit. We support ME/CFS and NEID patients through rigorous reporting, reliable information, effective advocacy and the provision of online services which empower patients and help them to cope with their isolation.
There are many ways you can help Phoenix Rising to continue its work. If you feel able to offer your time and talent, we could really use some more authors, proof-readers, fundraisers, technicians etc. We’d also love to expand our Board of Directors. So, if you think you can help in any way then please contact Mark through the Forums.
And don’t forget: you can always support our efforts at no cost to yourself as you shop online! To find out more, visit Phoenix Rising’s Donate page by clicking the button below.
View the Post on the Blog
The WHO ICD featured recently in an online article (since withdrawn), which heightened patient concern over what might happen when the current ICD-10 is finally revised. N.A.Wright provides a timely summary of this international classification system, considers some of the issues surrounding the existing and proposed listing, and calls on our advocacy organisations to get involved...
The World Health Organization (WHO) is responsible for producing an International Classification of Diseases – the ICD.
An important document in standardising epidemiological data, the ICD has often been a source of confusion in discussions about ME/CFS.
The ICD is subject to continuous review with updates published annually and major revisions are intended to be produced every ten years. The date for publication of the ongoing full revision has recently been announced as 2017, providing a three year extension to the formal revision process that began in 2007.
Understanding what the ICD is, what its limitations are and how best to engage with the revision process should be a significant focus for ME/CFS advocacy.
The ICD through an ME/CFS Lens
Many ME/CFS patients first gained awareness of the World Health Organization International Classification of Diseases in the various online discussions that surrounded the UK PACE trial and the arguments made against PACE and its associated projects.
As part of the challenge to the PACE research a patient advocacy position was advanced which relied on the classification of ME as a neurological condition under the World Health Organization’s “International Classification of Diseases” (ICD).
This advocacy position can be summed up as, “ME is neurological because the World Health Organization says so”. Unfortunately, it is a position that is poorly founded because the ICD simply does not confer the authority that is implied.
Equally unfortunate is that the WHO itself perhaps overstates its own case by claiming on its website that, “The International Classification of Diseases (ICD) is the standard diagnostic tool for epidemiology, health management and clinical purposes.”
The ICD has very limited clinical application or diagnostic power, and with the exception of Mental Health (see 'Limitations of the ICD' below), has no significant diagnostic role in the health delivery systems of most developed countries.
A far more accurate statement of what the ICD is and what it can be used for, is to be found on the NHS Connecting for Health website:
“ICD-10 is a statistical tool that requires adherence to and application of specified definitions and rules to enable accurate, consistent and comprehensive capture of data for secondary purposes which is undertaken by health informatics professionals – clinical coders.”
A Brief History of International Disease Classification
International disease classification began a century before the United Nations (UN) and WHO came into existence. Building on the work of the British Registrar General from 1837, the first international listings of causes of mortality were accepted by the International Statistical Congress in 1855 and it is from this that the ICD revision numbers commence, the current publication is ICD-10.
By 1900 mortality statistics were augmented with a classification of morbidity by disease and further revisions saw, with the inception of the UN, the adoption by WHO of ICD-6, in 1946. Subsequent revisions were envisaged to take place every 10 years, although slippage at various stages leaves the current published revision at ICD-10 .
ICD-10 is currently under revision and will be replaced by ICD-11, which is scheduled for World Health Assembly approval in May 2017.
The term Benign Myalgic Encephalomyelitis was first included in ICD-8 which was published in 1969 where it was categorised under the heading “Disorders of the Nervous System” with the coding number G93.3. This classification was repeated in ICD-9 (published in 1975) and in ICD-10 (published in 1992).
The replacement for ICD-10 is long overdue and it must be expected that after more than 20 years, as part of the general updating process, some reconsideration of the classification of ME may take place.
Limitations of the ICD
Although vastly more sophisticated than envisaged by the pioneers of international disease statistics, the ICD is still primarily only a system of categorisation which to date has not been a reference of internationally agreed diagnostic criteria.
This may to some extent change with ICD-11 where the inclusion of diagnostic criteria may appear as part of the disease descriptors. There is one part of the ICD which has long standing acceptance as having diagnostic authority, that is Chapter 5: Mental and Behavioural Disorders, which is published in two separate editions, the Blue Book: Clinical Descriptions and Diagnostic Guidelines and the Green Book: Diagnostic Criteria for Research.
The ICD can be compared to the Dewy Decimal System (DDS) which is used throughout the world to give structure to libraries. Just because a book is allocated a given DDS number does not mean that the book lacks characteristics which may see it placed in another category, or that at some future date the category to which that particular book may have been assigned, may have its description changed or be further subdivided.
The book will not change but its system number and place on the shelf might.
The direct comparison between the ICD and the DDS is limited because diseases are not single edition books; research and developments in treatment mean that ‘diseases’ are subject to constant updates and even to full re-writes as well as the production of multiple volumes which may cross categories.
So, unlike a library, not only are the categories within the ICD subject to change, but so also is the material that is contained within the categories. This is why in addition to annual internal updating via the WHO-FIC Committees, there is a notional ten year process of open review; it is understood that for the ICD to remain relevant it must be constantly globally updated.
The fact that ICD-11 is already 12 years late is no doubt evidence of the huge task that this updating represents in the face of unprecedented world wide investment in health research.
In summary, what this means for ME/CFS advocacy is that categorisation within the system has not conferred diagnostic authority and the location of a disease in a particular category only defined what was seen as useful from the perspective of gathering data, at a particular time.
ICD categorisation will always be subject to change, using the ICD as though it were a fixed and authoritatively determined diagnostic statement, rather than a serviceable means of data recording, may not be advisable from an advocacy perspective.
ICD Clinical Modifications
International Classification of Diseases-Clinical Modifications (ICD-CM), are nationally specific adaptations of the ICD categorisation system which may include diagnostic and clinical detail, such that an ICD-CM can be used as a diagnostic and clinical reference within a specific nation’s health provision. ICD-CMs should not be confused with the ICD.
At least 12 countries including the US, Canada, Australia and Germany, employ ICD Clinical Modifications, which serve a variety of purposes in different countries. The US, for example, has a sophisticated process overseen by the Centers for Medicare and Medicaid Services.
Clinical Modifications, although based strictly upon the ICD categorisation, unlike the ICD itself, do have direct clinical relevance for health provision in each relevant country. Though it is important to be clear that updates to the ICD, may not feed directly into the national ICD-CMs.
Each national ICD-CM is subject to national review which may substantially lag behind changes to the ICD. The US in particular trails behind much of the rest of the world by still using a Clinical Modification based on ICD-9, a version long since retired by WHO. ICD-9-CM does have an annual process for updates, but the US doesn’t plan to shift from ICD-9-CM to ICD-10-CM until late 2014.
International Classification of Diseases 11th Revision
The International Classification of Diseases (ICD) 11th Revision is a currently active process, and it is this process that will produce the documents which will be collectively known, once approved by the World Health Assembly, as ICD-11.
According to the WHO:
“ICD-11, is now being prepared. The development phase will continue for three years and ICD-11 will be finalized in 2017. For the first time, through advances in information technology, public health users, stakeholders and others interested can provide input to the beta version of ICD-11 using an online revision process. Peer-reviewed comments and input will be added through the revision period. When finalized, ICD-11 will be ready to use with electronic health records and information systems. WHO encourages broad participation in the 11th revision so that the final classification meets the needs of health information users and is more comprehensive.”
Participation is additionally invited and public health users, clinicians, researchers and other stakeholders can register to provide input into the drafting process and to assist in support activities, such as participation in field tests and translations.
Access and the registration portal is here: ICD-11 Beta Draft (or click the image above).
While open to individuals, achieving effective influence will almost certainly need the force of established organisations supported by acknowledged medical expertise. Co-ordinated action by a coalition of such organisations would be the ideal.
ME/CFS and ICD-11
Because they affect diagnosis and treatment provision directly, the various national ICD Clinical Modifications have the most immediate impact upon patients. Nevertheless the positioning of ME/CFS within the ICD system as a whole is important because such an international reference can influence the context in which the illness is considered in terms of research and health service resource allocations, across the globe.
Changes to the structure and chapter organisation between ICD-10 and ICD-11 will mean that many ICD terms will be presented differently. A new code numbering system applies across the entire classification, so the current coding position of G93.3 for Benign Myalgic Encephalomyelitis, is likely to change, though categories with ICD-10 equivalent terms will be cross referenced to the current ICD-10 codes. Some parent class terms are being retired and there are also proposals for changes to category hierarchies.
In early 2013 the proposal displaying in the Beta drafting platform was to make CFS the ICD Title code, with Benign Myalgic Encephalomyelitis specified as the Inclusion Term to CFS; and PVFS listed under Synonyms to CFS. There will be significantly more textual content across all chapters of ICD-11 and all ICD Title codes will be allocated Definitions and selected other "Content Model" descriptors.
Patient advocacy groups need to monitor these developments and to seek to influence, not just the working proposals on chapter location and hierarchy, but to also ensure that proposals for definitions and other textual content reflect the long term interests of patients.
Dx Revision Watch makes the following interesting observation:
“Unlike ICD-10, multiple parents are allowable under ICD-11: TAG Neurology may intend to assign one or more of these terms to multiple parents within the same chapter, or to code to parents located under more than one chapter, for example, under parent classes, Symptoms, signs and clinical findings involving the nervous and musculoskeletal system or Functional disorders of the nervous system (located under both Chapter 07 and Chapter 19), ...”
It would certainly be a pragmatic approach to have ME/CFS under multiple listings. While epidemiological data collection would be somewhat complicated, multiple listings would allow the accommodation of future nomenclature changes relative to developments in research and treatment.
Future Work
Through her website, Dx Revision Watch, Suzy Chapman has been monitoring and reporting on the progress of the revision to PVFS (Post Viral Fatigue Syndrome), BME (Benign Myalgic Encephalomyelitis) and CFS (Chronic Fatigue Syndrome) for ICD-11 for the last five years. Suzy has also monitored and reported on the revision of the ICD-10 and DSM (Diagnostic and Statistical Manual of Mental Disorders) Somatoform disorders.
However, Suzy has recently announced that for personal and political reasons she is stepping back from the work she does via her site. She does not anticipate publishing and circulating new content, although there will be some updates to existing reports.
The WHO is an international body: our reliance on a single volunteer in a single country to monitor and report on the ICD process for the global ME/CFS patient and professional population, has been neither fair, nor reasonable.
Suzy Chapman's stepping back should be seen as a wake-up call to patient and advocacy organisations to get involved.
ICD-11 need not be seen as inherently a threat to the interests of ME/CFS patients; however to make the most of the opportunities that the ICD-11 process offers, patient organisations must become active participants in the development of the ICD-11 draft over the next three years.
The first objective of that participation should be to ensure that the lack of transparency that currently affects the ICD-11 position on ME/CFS, (and to which patients have been alerted by Dx Revision Watch, see: A Beta draft black hole), is urgently resolved.
*note ME/CFS is used in this article as a generic term, it doesn’t imply any diagnostic preference.
**The author thanks Suzy Chapman for helpful comments and suggestions in relation to the ICD-11 revision process. All views expressed are the author’s own.
Phoenix Rising is a registered 501 c.(3) non profit. We support ME/CFS and NEID patients through rigorous reporting, reliable information, effective advocacy and the provision of online services which empower patients and help them to cope with their isolation.
There are many ways you can help Phoenix Rising to continue its work. If you feel able to offer your time and talent, we could really use some more authors, proof-readers, fundraisers, technicians etc. We’d also love to expand our Board of Directors. So, if you think you can help in any way then please contact Mark through the Forums.
And don’t forget: you can always support our efforts at no cost to yourself as you shop online! To find out more, visit Phoenix Rising’s Donate page by clicking the button below.
View the Post on the Blog