roller
wiggle jiggle
- Messages
- 775
the pressure, not really the oxygene
@LHCTom
Still trying to get my head around your medical history. There is no question your metabolism is way out in left field. You do look like a classic case of Naviaux's hypometabolic state. What else is going on is a real question, and unfortunately, there are way too many possible causes.
Yes its a mess! But why is the question.
In terms of infectious agents, I see spirochetes, intestinal bacteria, parasites, fungi and yeast. I did not see mention of toxoplasma gondii, but the association with cats makes that a possibility. I would not be surprised to see high titers of viral antibodies, if your immune system were in good condition, which I doubt considering those multiple infections. I wouldn't be surprised if your immune system has been throttled down to avoid autoimmune disease.
Yes I'm IgG but not IgM positive for toxoplasma Gondii. Just around the time I first began struggling I had been given a feral kitten. Feral kittens being wild are common carriers of Toxoplasma Gondii and Bartonella. Toxoplasma Gondii is a lifelong infection and I've tried to convince a number of doctors including Montoya of Stanford to look harder for Toxo. Montoya is among the world's leading experts in Toxo but my view is expertise makes for lack of creativity. I have leaky gut and its caused about a dozen food allergies including my favorite foods. My total IgE can run over 1000 and my IL4 quite high which creates a Th2 immune system bias at the expense of TH1. I was also treated at least 10 times with Prednisnone and that plus the TH2 bias qualify me as partially immune compromised. My total IgG runs abnormally low. I also see a high EOS on about every third CBC.
I have a pulse oximeter that I run all night and it shows my O2 saturation rarely goes below 90%. Yet when I awake, I feel hypoxic or hypercapnic. I have a brand new CPAP machine which does not help one bit. The CPAP is over-coming any apnea events and reports its working well. So my cells seem to not be getting O2 yet my O2 saturation and CPAP failure suggest its not my respiration alone. That implies my blood is being oxygenated but its not being delivered to my cells while I sleep. When you sleep, your respiration is depressed and the O2 saturation declines but not enough to cause a problem unless something else is interfering like a parasite. When I was tested for Lyme at Fallon's Tick Borne research Center at Columbia and again by 2 integrative doctors via IGenex, I also tested positive for Babesia Duncani. So I was treated with Mepron and Arithromycin.
So I'm very sispicious that something is effecting my blood flow through my capillaries while asleep and my O2 saturation is 90%. On this hypothesis, I switched to my old blood pressure medication Lisinopril ( ACE inhibitor) and Amlodipine ( Calcium Channel Blocker) and away form a beta blocker. I also added a baby aspirin and L-arginine in an attempt to maximize blood flow and minimize blood vessel constriction. That greatly reduced my awakening symptoms. So the question is why? Is it a blood parasite that is further limiting my O2 carriage in my blood or causing something like Rouleaux which is where red blood cells stack due to electric charge which makes them flow less easily and congesting capillaries. I was also IgG positive for Mycoplasma Pn. which is another possibility along with the Toxoplasma, Babesia, 2 fungus's ( Scedosporium apiospermum and Candida guilliermondii), Lyme and I was culture positive for MRSA. I was ALS culture positive for Lyme 3 times, CDC positive by iGenex once, 4/10 IgG by Stony Brook Lab, and Immunetics C6 positive by iGenex, Stony Brook Lab and Quest.
Something on this list is interfering with the delivery of O2 to my cells which cannot be overcome by CPAP and a finger pulse oximeter suggests my saturation is not all that bad.
That foot drop at the onset is a clear sign of some neurological problem, but what? MS?
That was 15 years ago but I believe it was when this all started.
If we are considering unusual infectious agents affecting both nerves and immune response I would wonder about HTLV. I'm sure you've been tested for HIV, but testing for HTLV remains rare, and usually depends on antibody response, which seems to be impaired.
Been tested for HIV 4 times negative but not HTLV.
("We've narrowed things down. It's either an RNA virus, a DNA virus, a retrovirus, a spirochete, a bacillus, a parasite or two, fungi or yeast.")
Some clusters of symptoms and signs you mention go along with mast cell activation disorders, particularly that Imidazoleacetic Acid being way out. Have you had other tests specific to mast cell function? This looks like a case of chronic immune activation firing in many directions.
I probably do have a mast cell activation disorder since certain drugs like Ibuprofen immediately trigger angio-edema.
Other patients I've heard from with that range of gut problems, sleep disorders, etc. have inherited connective tissue disorders. These can range from rare (EDS) to extremely rare (HKPP). That last is connected with a potassium channelopathy. Many have had surgery to reduce apnea, and quite a few of these were not completely successful. Do you have trouble swallowing at present?
I had a sleep study at Stanford and they found mild sleep apnea back in 2003. I had surgery in 2008 and it greatly improved. Its partially come back but the good O2 saturation and the CPAP does not correct for my hypoxic-like awakenning suggesting its not sleep apnea but that could be an aggravating factor for a red blood cell parasite.
You have described a complex case with multiple layers of pathology. If present day medical professionals can't get to the bottom we need a new generation of doctors. Something is obviously wrong.
I've been through every doctor at Kaiser and then multiple Stanford doctors, numerous integrative doctors and now I'm seeing a UCSF Infectious Disease Doctor. I was referred by a UCSF Nephrologist. My creatinine and Ck go up and down together. My creatinine goes as high as 2.1 ( kidney disease) but then falls to 1.1-1.2 after I'm treated with antibiotics. Go figure. When my awkenning with confusion,sever pain, high BP, headache, need for air etc.. was only episodic ( every 3-4 months), I was able to stop it with Bactrim. None of the doctors believed me and others said it couldn't be its antibiotic affect. It turns out Bactrim is a folate synthesis inhibitor and has some effectiveness on Toxoplasma Gondii and Fungus besides bacteria such as Bartonella.
As always I am not a medical doctor, and the opinions I express are merely my own.
The stated range in at least two of the labs I have handy is 22 to 29, and I have been coming in pretty consistently at 21 or 22. I've been flagged as out-of-range low at least three times in the last 18 months.
I don't hyperventilate, and I am amused when ME/CFS experts throw that out there (I've had three solid experts offer that). Imo, it holds about as much merit as my OI is caused by stress.
Thanks for the insights. I will see if I can wrap my head around the math. Doubtful. I do so out of curiosity, not under any illusions you are a doctor, and I also am appreciative of your input with that understanding.
The stated range in at least two of the labs I have handy is 22 to 29, and I have been coming in pretty consistently at 21 or 22. I've been flagged as out-of-range low at least three times in the last 18 months.
I don't hyperventilate, and I am amused when ME/CFS experts throw that out there (I've had three solid experts offer that). Imo, it holds about as much merit as my OI is caused by stress.
Thanks for the insights. I will see if I can wrap my head around the math. Doubtful. I do so out of curiosity, not under any illusions you are a doctor, and I also am appreciative of your input with that understanding.
Yes, it's me from the Lymenet forum. Still dueling over there with IDSA , NIH and ALDF types. Let me dig around and get you those values.
Hey LHCTom - my C6 is still rising....
Here's two, @LHCTom , one from 2015 and one from 2016.
2015:
CO2 = 19 range: 22-29
Potassium = 4.0 range: 3.3-5.3
Chloride = 101 range: 96-108
Sodium = 138 range: 133-145
2016
CO2 = 20 range:23-32
Potassium = 4.3 range 3.3-5.5
Chloride = 103 range 90-108
Sodium = 142 range 136-146

The fact that hyperbaric oxygen therapy (HBOT) does not help ME/CFS very much seems to indicate that oxygen shortage is not the issue in ME/CFS.
Hyperbaric oxygen therapy (HBOT) uses high ambient pressures of up to 3 atmospheres to dissolve more oxygen into the water component of your blood. HBOT increases the amount of dissolved oxygen by a factor of around 20 times, meaning that with HBOT, up to 30% of the oxygen carried in your blood is oxygen dissolved in the water, and the other 70% is hemoglobin-bound oxygen carried by red blood cells. More info in this post.


I don't hyperventilate, and I am amused when ME/CFS experts throw that out there (I've had three solid experts offer that). Imo, it holds about as much merit as my OI is caused by stress.
Telling you that its caused by hyperventillation is beyond absurd, its stupid! Where has creativity gone - under a rock!
Your red blood cells hemoglobin must be able to accept the O2 provided by HBOT and if not, HBOT will not help.
If your red blood cells accept adequate O2 and your Co2 evacuation is also adequate, your circulation at the capillary level could prevent cell <-> CO2/O2 exchange. Ther are a number of parasites that infect the red blood cells and interfere with delivery of O2 and CO2 exhaust even when HBOT offers excessive O2 at the level of the lungs.
Some conditions cause Rouleaux (singular is rouleau) which are stacks or aggregations of red blood cells (RBCs) which form because of the unique discoid shape of the cells in vertebrates. The flat surface of the discoid RBCs gives them a large surface area to make contact with and stick to each other; thus forming a rouleau. The Rouleaux looks like stacks of red blood cells somewhat like stacked coins. They stick together due to an innapropriate electric charge that can be a result of infections or other conditions. These stacks essentially congest your capillaries reducing blood flow and O2/CO2 exchange.
I was diagnosed with Chronic Fatigue by multiple doctors including one at Stanford, OMI, multiple integrative clinics, Kaiser among others. But even though my symptoms match the criteria, other symptoms do not. I was one of the patients in Dr. Naviaux’s recent metabolomics CFS study and helped fund it. It can be found at http://www.pnas.org/content/113/37/E5472.full . My metabolic abnormalities fell inside the identified biomarker signature including the following abnormalities:
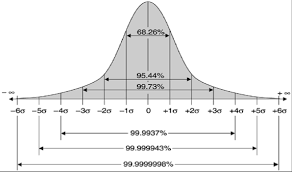
I had a total of 28 metabolic abnormalities defined by outside 2 SD above or below normal. A common theme seen in some of my symptoms and abnormalities is a gut microbiome dysbiosis and a leaky gut epithelium.
1) L-Carnitine was 2.1 SD below the mean and several acyl-carnitines were increased 1.7-2,5 above the mean suggesting decrease fatty acid oxidation in mitochondria is decreased.
2) Phosphatidyl Choline lipids were 2-2.3 SD below normal
3) Sphingomyelin lipids were decreased 2.2-2.8 SD below normal
4) Homoserine was 2.0 SD below the mean
5) Betaine was 3.0 SD below the mean
6) DHEA Sulfate was 2.5 SD below the mean
7) CoQ10H2 and CoQ9H2 were decreased 1.5 to 4.0 SD below the mean suggestive of CoQ10 deficiency
8) Imidazoleacetic Acid ( IZA) was 3.7 SD below the mean. Consitent with chronic histamine release and consitent with chronic basophil and mast cell histamine release and allergic activation – Consistent with my having at least a dozen testing confirmed IgE mediated food allergies
9) Lathosterol was 2.1 SD below the mean. Consistent with decrease in de novo cholesterol synthesis.
10) Elevated plasma sucrose, phenyllactate and a decrease in several bile acids ( glycocholic and taurocholic ) which is consistent with a relatively leaky gut epithelium. This is consistent with the extensive food allergies due to the leaky gut.
11) Homovanillic Acid was decreased 1.9 SD suggesting a mild dopamine deficiency.
One of the problems I see in all people with Chronic Fatigue Syndrome is the vague symptoms which overlap with a multitude of conditions. Fatigue is among the most common symptoms from nearly a hundred different conditions. This suggests there may be many underlying pathologies to CFS/ME yet most people receive one diagnosis which has no known cause and no reliable treatment. Different people and studies have seen improvements due to a variety of treatment but they typically do not apply widely. This is the frustration of CFS/ME.
I’ve pursued a diagnosis of an underlying pathology irrespective of how a CFS/ME diagnosis discourages many doctors from pursuing a deeper analysis. I have recently had my symptoms reach an acute stage that I believe has now presented me with a “lead” that is a solid as finding DNA at a crime scene. Most of the “leads” in the past have been analogous to an eye witness without their glasses in the dark. I’m curious if I’m alone as there have been “hints” that this now acute problem has been there from the beginning over 10 years ago. I'm telling this story in hopes it triggers ideas in other.
From the very beginning in the late 90's, I always knew that my fatigue and a raft of other symptoms all seem aggravated while asleep. I would awake feeling the worst and it would take until around noon before I felt well enough to function. Then this cycle would repeat the next night and on and on for more than a dozen years. I experienced bouts of pain, sweats, nausea, low grade night fevers ( 99-100.5), swelling, numbness, etc.. but the pattern kept evolving and changing. Only the sleep trigger, fatigue, felling ill and pain in the morning were truly constant. It all started with a bout of foot drop followed by numbness up my legs, the discovery I produced no testosterone, had high CK=250-700, high total IgE=400-1100, and wildly varying creatinine (1.1->1.4->1.2->1.6->1.3 2.1->1.6->1.4->1.12) seemingly going down after antibiotic treatment. Very suspicious.
I had a sleep study at Stanford which found mild sleep apnea. I used CPAP for 2 years followed by surgery at Stanford which seemed to stop all O2 desaturations. I then went on to be diagnosed with Lyme and Babesia as I live one 35 acres which are infected with ticks. I Helped fund a few studies by Dr. Bob Lane of UCB and we collected about 100 nymphal ticks on my property within 100 feet of my home and found both B burgdorferi and B. miyamotoi described here: http://wwwnc.cdc.gov/eid/article/22/12/15-2046_article . I have been bitten numerous times by ticks over 20 years and was CDC and IGenex positive on the WB plus C6 positive. A Babesia IFA was both IgG and IgM positive. I wasn’t sure what to believe so I went to Dr Fallon’s Tick Borne Research Center at Columbia for a second opinion.
They confirmed the positive C6 ELISA at Stony Brook Lab and I had 4/10 antibodies on the WB which fell short of the CDC 5/10. They said it was likely I had Lyme due to the positive C6 and 4/10 near CDC positive that was consistent with the IGenex testing. I also had a positive Babesia Microti IgM positive ELISA by Medical Diagnostics Laboratories while at Columbia. I returned and was treated with antibiotics orally for 1 year followed by Mepron plus arythromycin for Babesia for about 6 months. I felt better but not great. I remained C6 ELISA positive until early 2015 after being tested each year until it became negative.
I noticed that every time I was given extensive antibiotic treatment, my creatinine and CK would decline to either normal or near normal. When I told doctors, they would dismiss this even though I graphed every creatinine and CK test from 2003 through 2016 and their correlation and antibiotic driven decline was obvious. Still not one doctor took this pattern seriously until recently. When they saw my creatinine drop, they were happy my kidneys were ok but never asked why my creatinine wildly fluctuated between about 1.1 and 2.1 in mysterious near synch with my CK muscle enzymes. I then investigated whether a fungal infection could be involved.
During the 2013 to 2015 timeframe, I had episodes of body pain focused in my hips and shoulders but also back and legs/arms where I could barely walk and felt like I had run a marathon in my sleep and awoke in this state. I was given prednisone by Kaiser which helped but worried me it could suppress my immune system should an infection be the real cause. One doctor believed it could be Bartonella due to my feral kitten and tick bites and we discovered Bactrim would stop the pain episode cold after about 4 days.
I then asked for both a fingernail and toenail culture and arranged multiple mycotoxin ELISAs. Bactrim is a folate synthsisis inhibitor and does have fungal effectiveness. The mycotoxin ELISAs came back positive 3 times. My fingernail culture came back with a “Scedosporium apiospermum” infection
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2223844/
and my toenails had a “Candida guilliermondii” infection. Its difficult to test for a disseminated fungal infection since once it reaches the blood, sepsis is not far away. Until a fungus breaks through the skin where it can be cultured, its hard to get at it if for example its in your muscles or kidneys.
So recently things have come to an acute “head” which puts the cause very closely related to my sleep as always suspected. But now when I fall asleep day or night, when I awake 30 minutes to 3 hours later, I feel confused, hypoxic in need of air, a severe headache, severe pain in my hips and shoulders and lesser pain throughout my large muscles. It was so bad I went to the ER where I was turned away since my most basic vitals were ok. So that points at respiration and or circulation. I utilized an overnight pulse oximeter which suggested my O2 saturation was rarely dropping below 90%. That would not explain such severe symptoms upon awakening. A sleep specialist suggested I use a snoring monitor APP on my phone which also indicated only mild snoring. I then tried CPAP and it too had NO effect. So that leaves excess CO2 due to failure to exhaust or circulation. My total CO2 or bicarbonate on metabolic panels was often near the top of the range and occasionally over. So was it an Acid/Base problem like respiratory Acidosis? My doctor arranged an Arterial Blood Gas test in the hospital and my PH was dead on normal and no blood gas abnormalities. CO2 is fleeting but it had no caused something like a Acid/Base disorder like Acidosis. The mystery deepens.
I saw a UCSF nephrologist since when I awoke, my BP was skyrocketing plus the unusual creatinine and CK behavior. My kidney was ok by ultrasound as was my kidney artery. He felt that since my creatinine comes down to normal regularly and my urine shows no protein and my ultrasounds were solid, it must be some underlying pathology such as an infection. He has referred me to a UCSF ID doctor and now my pattern and creatinine behavior is so specific, I believe we are closing in on the culprit. My personal suspicion at this point is I am experiencing a hypoxic condition while sleeping but its not due to respiration as much as the inability of my blood to accept “enough” O2 and flow through my capillaries while sleeping. This could also cause elevated CO2 since its removal from cells would also be affected by a combined oxygenation/blood flow problem. Now that I’m this focused, can I get a doctor to dig in properly.
To support this conjecture, I switched my blood pressure medication from metopronol ( a beta blocker ) back to my previous Lisinopril ( an ACE inhibitor) and Amlodipine ( a calcium channel blocker) plus a baby aspirin and L-arginine to ease blood flow and prevent my blood vessels from contracting thereby allowing O2 saturated red blood cells to flow. This has now reduced my night awakenings in a panic and in pain with HBP to almost nothing. But I still feel lousy in the morning so its not a full solution. But now I have the ability to manipulate the symptoms based on a hypothesis that was left after eliminating sleep apnea and an acid base disorder such as respiratory acidosis.
So why did I tell this story? I’m curious if any of this rings any bells with anyone else diagnosed with CFS? Failure to deliver adequate O2 to one's cells is a sure fire way to cause fatigue and a myriad of othre symptoms. I also wanted to show my example of where CFS does map to the metabolomics biomarker recently found in Dr Naviaux's study yet the underlying mechanism has to do with delivering inadequate O2 and or removing adequate CO2 from cells. No doubt failure to deliver adequate O2 to one cells and mitochondria would badly disrupt metabolism.
In my case, suspect this will be tracked to some kind of infection or autoimmune condition that is affecting my blood vessels and or capillaries and circulation - something like a vasculitis or similar condition. But my awake respiration and O2 delivery and CO2 removal are probably at an acceptable albeit marginal level. Only when I’m sleeping and my respiration depresses naturally and O2 saturation declines to the mid 90% range and when combined with some apnea events does my O2 delivery to cells fall over some cliff and become inadequate. I suspect I have had this going on chronically for a dozen years and something like the Prednisone treatment unleashed an infection or something similar happened that pushed it to an acute phase which may be understood by doctors. I hope.
Does this ring any bells or am I alone in this pattern?