View the Post on the Blog
The 2014 conference season began yesterday at Stanford, home of Dr. Jose Montoya and his team, and searcher was there to provide a live commentary on the presentations from an all-star line-up of clinicians and scientists and which featured some exciting new developments on the research front...
We will also aim to also publish a public article - such as this one - on each of the days following a conference, providing everyone with a chance to catch-up on events, and after the conferences are finished, we will look at more in-depth analyses of the presentations: once we have had a chance to digest all the information, perhaps interview some of those involved - and pause for breath!
The Stanford ME/CFS Initiative is the department run by Dr. Jose Montoya, a noted clinician and researcher, and well recognised by the patient community, and it was he who opened the conference - and about whose recent research there was perhaps most expectation by the patients in the audience and following at home.
Notes taken from the conference are highlighted below and click on the photographs to access a profile (if one was available).
Stanford CME Symposium Statement of Need
This CME Symposium seeks to fulfill the need in the medical and research community to increase the awareness that Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a physical condition and real disease.
With this activity we hope to impact the fund of knowledge that will optimize the medical care of ME/CFS patients by providing tools and resources from keynote speakers in proper diagnosis, evaluation and management of the ME/CFS patient, as well as spark new ideas for further research.
Yesterday's agenda can be read in full: HERE
Searcher 08.45:
“I arrived a little while ago. There are a lot of people milling around and the place appears to be packed to capacity. Most of the attendees appear to be doctors or professionals. I spoke with Dr Friedberg and he said that there a good number of people signed up for IACFS/ME.
“So far I have seen a lot of the well-known doctors and researchers in the CFS world, including Drs Peterson, Kogelnik, Friedberg, and Vernon.
“The organizers planned well and had golf carts to take us from cars to the front door of the building.
The Stanford ME/CFS Initiative:
A Brief History of Collaboration, Innovation and Discovery in the Field of Infection Associated Chronic Diseases

Jose G. Montoya, MD, FACP, FIDSA
Professor of Medicine, Division of Infectious Diseases and Geographic Medicine Stanford University School of Medicine
Director, Palo Alto Medical Foundation Toxoplasma Serology Laboratory
Searcher 09.15 - 09.40:
“Dr Montoya just started speaking...
“College, high school, and middle school students are going to be volunteering in the summer of 2014.
“He thanked the team and partners throughout the Department of Medicine, and the advisory board.
“He is walking through a case of a scientist who got a severe case of ME/CFS starting in 2006. It started with digestive problems. Other illnesses were ruled out. He had a high level of HHV-6A DNA in his blood and cerebrospinal fluid.
“The scientist (gender purposely not specified) improved after going on valcyte in 2009. But he or she just had a recent and major relapse.
“Unrelated side note: I am pretty sure I see Ashok Gupta.
“Dr. Montoya is going through symptoms, starting with the standard set (6 months of symptoms, viral symptoms.)
“He then says there are a lot of additional symptoms including gastrointestinal, cardiovascular/autonomic, neurological, etc.
“Illness involves several organs/systems, is chronic and fluctuating.
“He is talking about the valcyte research (all previously published.) He said it's not only an antiviral, it is also an immunomodulator (which wasn't even known by the antiviral makers.)
“He mentioned the Synergy trial. K-Pax helped patients with HIV, so they want to see if it helps people with ME/CFS. They want to confirm Dr Kaiser's results and that's a double-blind, randomized, placebo controlled trial.
“He is talking a lot about how it's important to do good scientific research. “Randomized, double-blind, placebo controlled clinical trials” and “Longitudinal Studies.”
“He is doing an intro on the cytokine findings [from his latest study]. I will ask during lunch if we can post about the findings.”
Epidemiology of ME/CFS, What Have We Learned?

Elizabeth R. Unger, MD, PhD
Chief Chronic Viral Diseases Branch
Division of High-Consequence Pathogens and Pathology,
National Center for Emerging and Zoonotic Infectious Disease Centers for Disease Control and Prevention
Searcher 09.45 - 10.40:
“Dr Unger is now speaking about epidemiology...
“She's talking about the "disagreement about terminology." There is honest disagreement and we need to agree on terminology. Several case definitions.
“Areas of consensus:
Health status in patients with chronic fatigue syndrome and in general population and disease comparison groups
[1996 Study referred to below]
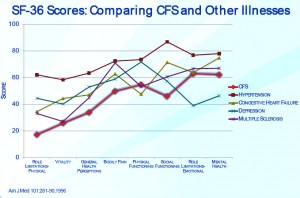
Patients and methods
The subjects of the study were patients with CFS (n = 223) from a CFS clinic, a population-based control sample (n = 2,474), and disease comparison groups with hypertension (n = 2,089), congestive heart failure (n = 216), type II diabetes mellitus (n = 163), acute myocardial infarction (n = 107), multiple sclerosis (n = 25), and depression (n = 502).
We measured functional status and well-being using the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36), which is a self-administered questionnaire in which lower scores are indicative of greater impairment.
Results
Patients with CFS had far lower mean scores than the general population control subjects on all eight SF-36 scales. They also scored significantly lower than patients in all the disease comparison groups other than depression on virtually all the scales. When compared with patients with depression, they scored significantly lower on all the scales except for scales measuring mental health and role disability due to emotional problems, on which they scored significantly higher.
“PEM or relapse is characteristic. Sleep problems, difficulty with memory or concentration, muscle and joint pain, dizziness, can be accompanied by other co-mobid conditions such as fibro, IBS, TMJ, MCS, etc.
“Key symptoms of the illness definitely interact:
“Areas of disagreement:
“Latinos>African Americans>Caucasians
“How common is ME/CFS? Pooled prevalence estimate is .31% in the US based on pop-based surveys. Range is .24-2.5% in 3 studies.
“Consistent finding in multiple studies.
“Showing chart about impairment vs other illnesses AM J Med 101:281-90,1996 by Komaroff. Worth looking at... [see box]
“Someone asked about 1-day vs 2-day exercise tests. They found that ME/CFS patients generally did poorly on 1-day tests so a 2-day test seemed needlessly onerous (not a quote).
Daily Fluctuations of Cytokines in ME/CFS Patients

Jarred Younger, MD
Assistant Professor in Pain Medicine
Director of the Adult and Pediatric Pain Lab at Stanford
Searcher 10.55 - 11.20:
“Dr Younger is talking about cytokine fluctuations. Patients have large symptom fluctuations (for example, from 20-80 on a 100 scale.)
“If a patient can get to 80, then it indicates they have the physiological capability to be at 80 all the time. He wants to find the cytokines that explain the difference.
“He tested patients 25 days in a row and had them track their symptoms. He's looked at fibromyalgia patients and ME/CFS.
“As most of us know from the publication, leptin was generally correlated with fatigue.
“Microglia are easily activated when exposed to different stimuli, such as infections, chronic stress. diesel fuel etc.. They also activated more easily with aging. Leptin also lowers threshold for microglia.
“The association with leptin opens up many treatment possibilities. More than Dr Younger could test in his lifetime.
“He listed a lot of meds (such as minocycline, naltrexone) that work on microglia. He also mentioned a lot of herbs (primarily Chinese) that have potential but haven't been studied.”
Gene Expression Findings in ME/CFS
Searcher 11.30 - 12.00:
“Dr. Kaushal is new to ME/CFS and finds it fascinating.
Lunch and Learn “Media Portrayal of ME/CFS”
Searcher 12.20 - 13.20:
“They are currently showing a showing a short version of Voices from the Shadows.
“I had not previously seen more than the trailer and it was incredibly moving (and infuriating.)
“Phil Bronstein is moderating, and the panel consists of David Tuller, Natalie Boulton (Voices from the Shadows), and Erin All Day (SF Chronicle).
“David Tuller is talking about how much the name affects the coverage of the illness. Everyone has fatigue, and people shorten the illness to "Chronic Fatigue." There's been a lot of effort for the name change.
“Voices from the Shadows is very powerful as is Laura Hilldebrand's piece. Unfortunately only patients and carers seem to have interest in the film, according to the producer Natalie Boulton.
“There is a lot of discussion in general about how bad it can be in the UK due to the psychiatric lobby. Simon Wessely comes up often
“It's obviously very hard for people who can't be active to be activists in the same way HIV patients were.
“Once XMRV was out of the picture journalists lost interest.
“A lot of attendees are asking questions about Lyme, but it's not a focus from the Stanford side as far as I can tell.
“Cardiovascular Aging in CFS”
Searcher 13.58:
“He first went through the previous cardio studies:
“One showed there was a trend toward reduced LV mass in CFS vs sedentary controls. Reduced stroke content as well. He thinks it's a decent study.
“Second study compared 4 groups: severe CFS, mild CFS, sedentary, and non-sedentary matched on gender and BMI. 15% decreased TBV account for 91-94% of the cavity volume difference. But, he seemed skeptical of some of the study design.
“His study had 3 groups: CFS (25), control: sedentary (26), control: highly active - really high bike score, mainly really active cyclists. (26) MFI-20 for patients: 78.7, for controls: 40.8:
“One doctor stood up to say that he had less patients than average develop cardiovascular disease.
MRI Findings in ME/CFS
Searcher 14.56:
“I need to confirm whether these results can be made public as I think they haven't been published yet. If so I will post as soon as I know.
“This session was focused on anatomical brain structure.
Quantitative EEG Studies Suggest Subcortical Pathology in ME/CFS

Marcie Zinn, PhD (pictured)
Research Consultant in Experimental Neuropsychology and Quantitative Electroencephalography, Stanford University Medical Center, Department of Infectious Diseases and Geographic Medicine
Executive Director, Society for Neuroscience and Psychology in the Performing Arts, Performing Arts Psychophysiology Research Institute
Searcher 17.05 (following permission obtained after presentations):
“So far I have found their findings to be the most fascinating of the conference because I am always curious about what is occurring in the brain when we experience "brain fog." I will speak with them more at IACFS/ME.
The following is a summary of Dr. Marcie Zinn's talk:
“They looked at the EEG of patients and controls to see if the Peak Alpha Frequency could help them differentiate patients and controls.
“CFS-patients produced significantly reduced PAF’s (Peak Alpha Frequencies) over 58% of the cortex compared to controls.
“PAF predicted MFI-20 fatigue (lower peak alpha frequency=>higher fatigue scores).
“Implications of these results:
“EEG can’t be used to diagnose ME/CFS yet but it can be used to evaluate the extent and nature of the brain dysregulation.”
This is a summary of Dr Mark Zinn's talk:
Anthony L. Komaroff, MD
The Simcox-Clifford-Higby Professor of Medicine, Harvard Medical School
Senior Physician, Brigham and Women’s Hospital
Searcher 15.30 - 16.10:
“Age: Average Mid-30s. Sex: 65% female (but note that women seek health-care more often than men on average).
“Socioeconomic: Middle-class, but more common among African-American/Latino minority populations on population-based surveys.
“Education: 50% college grads in office-based samples.
“Only common physical examination abnormality was posterior cervical adenopathy at 35%-45% and impaired serial 7's at 30-40%
“He showed the same chart from the 1996 study I earlier mentioned which indicated that CFS patients had worse functioning than any other group he studied.
Dr Komaroff's summary:
Evidence of CNS Involvement in CFS:
“Great comment from an audience member (a Phoenix Rising member) about CBT:
“He's finishing by going through treatments. It's the standard list of sleep meds, CBT to deal with symptoms, GET very carefully done.
“There is extensive research to show differences between patients and controls.
“An audience member asked about TMS. He hasn't tried it and doesn't know of any studies on it. He thinks anecdotally 50% of patients have some response, but he doesn't know of anyone who had a strong response.
“Circulating Cytokines in ME/CFS Patients Reveal a Novel Inflammatory and Autoimmune Profile”

Jose G. Montoya, MD, FACP, FIDSA
Professor of Medicine, Division of Infectious Diseases and Geographic Medicine Stanford University School of Medicine
Director, Palo Alto Medical Foundation Toxoplasma Serology Laboratory
Searcher 17.10:
“Dr Montoya's talk. With much thanks to a fellow patient, Epiphany, for assistance and note-taking
“The following relates to his latest study:
“1. They measured 51 cytokines at the same time, 2 serums taken 2/day to control for variations
“2. Two-sided independent t-test, linear regression, linear regression, LASSO method
“3. Cytokines are a highly interconnected network, so very complicated
“4. Healthy control cases (similar ages, gender distribution, PEM was present in 96% of patients who met the Fukada criteria):
“6. 13 cytokines related (these were identified as increasing with CFS severity): related to the following responses: cell trafficking, cell activation, cell growth and differentiation, cytokine production, Th1 v. Th2 responses
“7. IL-17 = cytokine associated with autoimmune disease (RA, IBD, MS); 2 cytokines are also highly associated with females
“8. Patients are more likely to have illness for longer with lower TGF-B levels (a powerful anti-inflammatory cytokine)!
Microbial Diagnostics and Discovery in ME/CFS

W. Ian Lipkin, MD
John Snow Professor of Epidemiology and Director Center for Infection and Immunity Mailman School of Public Health
Professor of Pathology and Neurology College of Physicians & Surgeons Columbia University
Searcher 17.25:
“Most diseases have origins in animals, not humans.
“Most important person in identifying a pathogen is the clinician, not the laboratory.
“He is showing a slide called "Models for Bacterium-triggered mental illness: CNS autoantibodies in mice exposed to group A Steptococci"
“The slide shows a video of a mouse doing compulsive behaviors. The researchers can see the antibodies in the mouse brains after autopsy which can also be seen in humans.
“Toxins can also lead to antibodies.
“Their hypothesis is that Kawasaki's disease is caused by an autoimmune reaction to candida in the troposphere.
“HIV patients who don't respond well to anti-retrovirals have high cytokines in reaction to pathogens. Prevotella seems like a key culprit and may need to be treated
“Chronic Fatigue Initiative Plasma Study (recent study as reported in 'Lipkin finds biomarkers not bugs', last year):
“Dr Fletcher said they have a grant to study microbrial translocation in ME/CFS. They will look at 4 timepoints over 18 months.
The End.
Searcher, summing up...
“I can't write much of a summary because I am super-fried but here's a short one:
“There were hundreds of attendees. They needed to move us to a bigger room because the regular room was standing-room only. I met a lot of patients, researchers, ME/CFS focused clinicians, and general physicians who see ME/CFS patients on occasion.
“The conference was super-intense. There were few breaks and even lunch had the Voices from the Shadows screening and the journalism talk.
“They had a lot of information to fit in one day, which is a great sign that Stanford is doing a wide-range of research with potential impact.
“There is, not surprisingly, frustration that there is not more funding to do research.
“Many of the who's who of ME/CFS research seemed to be there. In no particular order and not including everyone, I saw Dr Montoya, Dr Kogelnik, Dr Byron Hyde, Dr Peterson, Dr Klimas, Dr Fletcher,Dr Vernon,Dr Komaroff,Dr Friedberg, Anne Whittemore, Carol Head (head of CAA).
“There is some overlap with IACFS/ME (like Lipkin and the Zinns) so we should have additional info then.”
Phoenix Rising is a registered 501 c.(3) non profit. We support ME/CFS and NEID patients through rigorous reporting, reliable information, effective advocacy and the provision of online services which empower patients and help them to cope with their isolation.
There are many ways you can help Phoenix Rising to continue its work. If you feel able to offer your time and talent, we could really use some more authors, proof-readers, fundraisers, technicians etc. We’d also love to expand our Board of Directors. So, if you think you can help in any way then please contact Mark through the Forums.
And don’t forget: you can always support our efforts at no cost to yourself as you shop online! To find out more, visit Phoenix Rising’s Donate page by clicking the button below.
View the Post on the Blog
The 2014 conference season began yesterday at Stanford, home of Dr. Jose Montoya and his team, and searcher was there to provide a live commentary on the presentations from an all-star line-up of clinicians and scientists and which featured some exciting new developments on the research front...
Stanford plays host to the first of five conferences over coming days, and, thanks to our volunteer 'searcher', all members of Phoenix Rising will be able to follow events as they unfold, live, in the members-only forum, and also with highlights via Twitter.
We will also aim to also publish a public article - such as this one - on each of the days following a conference, providing everyone with a chance to catch-up on events, and after the conferences are finished, we will look at more in-depth analyses of the presentations: once we have had a chance to digest all the information, perhaps interview some of those involved - and pause for breath!
The Stanford ME/CFS Initiative is the department run by Dr. Jose Montoya, a noted clinician and researcher, and well recognised by the patient community, and it was he who opened the conference - and about whose recent research there was perhaps most expectation by the patients in the audience and following at home.
Notes taken from the conference are highlighted below and click on the photographs to access a profile (if one was available).
Stanford CME Symposium Statement of Need
This CME Symposium seeks to fulfill the need in the medical and research community to increase the awareness that Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a physical condition and real disease.
With this activity we hope to impact the fund of knowledge that will optimize the medical care of ME/CFS patients by providing tools and resources from keynote speakers in proper diagnosis, evaluation and management of the ME/CFS patient, as well as spark new ideas for further research.
Yesterday's agenda can be read in full: HERE
Searcher 08.45:
“I arrived a little while ago. There are a lot of people milling around and the place appears to be packed to capacity. Most of the attendees appear to be doctors or professionals. I spoke with Dr Friedberg and he said that there a good number of people signed up for IACFS/ME.
“So far I have seen a lot of the well-known doctors and researchers in the CFS world, including Drs Peterson, Kogelnik, Friedberg, and Vernon.
“The organizers planned well and had golf carts to take us from cars to the front door of the building.
“The food is a gluten-lovers paradise  There is fruit though...
There is fruit though...
The Stanford ME/CFS Initiative:
A Brief History of Collaboration, Innovation and Discovery in the Field of Infection Associated Chronic Diseases
Jose G. Montoya, MD, FACP, FIDSA
Professor of Medicine, Division of Infectious Diseases and Geographic Medicine Stanford University School of Medicine
Director, Palo Alto Medical Foundation Toxoplasma Serology Laboratory
Searcher 09.15 - 09.40:
“Dr Montoya just started speaking...
“College, high school, and middle school students are going to be volunteering in the summer of 2014.
“He thanked the team and partners throughout the Department of Medicine, and the advisory board.
“He is walking through a case of a scientist who got a severe case of ME/CFS starting in 2006. It started with digestive problems. Other illnesses were ruled out. He had a high level of HHV-6A DNA in his blood and cerebrospinal fluid.
“The scientist (gender purposely not specified) improved after going on valcyte in 2009. But he or she just had a recent and major relapse.
“Unrelated side note: I am pretty sure I see Ashok Gupta.
“Dr. Montoya is going through symptoms, starting with the standard set (6 months of symptoms, viral symptoms.)
“He then says there are a lot of additional symptoms including gastrointestinal, cardiovascular/autonomic, neurological, etc.
“Illness involves several organs/systems, is chronic and fluctuating.
“He did a shout-out to patients who are bedbound. Seeing these patients makes him realize that curing ME/CFS is urgent...
“Why did Stanford get involved in CFS? In response to the suffering experienced in solitude by millions of patients who have patiently waited for an answer from the medical and scientific research communities.”
“He is talking about the valcyte research (all previously published.) He said it's not only an antiviral, it is also an immunomodulator (which wasn't even known by the antiviral makers.)
“He mentioned the Synergy trial. K-Pax helped patients with HIV, so they want to see if it helps people with ME/CFS. They want to confirm Dr Kaiser's results and that's a double-blind, randomized, placebo controlled trial.
“It's standing-room only now and they are opening up an overflow room...
“He is talking a lot about how it's important to do good scientific research. “Randomized, double-blind, placebo controlled clinical trials” and “Longitudinal Studies.”
“He is doing an intro on the cytokine findings [from his latest study]. I will ask during lunch if we can post about the findings.”
“Our goal is for healthcare providers worldwide to acknowledge that CFS and Chronic Lyme Disease are real diseases; thus, validating patients and fully integrating them back into mainstream” Dr. Montoya (see a summary of the Stanford research HERE)
Epidemiology of ME/CFS, What Have We Learned?

Elizabeth R. Unger, MD, PhD
Chief Chronic Viral Diseases Branch
Division of High-Consequence Pathogens and Pathology,
National Center for Emerging and Zoonotic Infectious Disease Centers for Disease Control and Prevention
Searcher 09.45 - 10.40:
“Dr Unger is now speaking about epidemiology...
“She's talking about the "disagreement about terminology." There is honest disagreement and we need to agree on terminology. Several case definitions.
“Areas of consensus:
“Severe fatigue, unexplained, not relieved by test, reduces activity.”
Health status in patients with chronic fatigue syndrome and in general population and disease comparison groups
[1996 Study referred to below]
Patients and methods
The subjects of the study were patients with CFS (n = 223) from a CFS clinic, a population-based control sample (n = 2,474), and disease comparison groups with hypertension (n = 2,089), congestive heart failure (n = 216), type II diabetes mellitus (n = 163), acute myocardial infarction (n = 107), multiple sclerosis (n = 25), and depression (n = 502).
We measured functional status and well-being using the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36), which is a self-administered questionnaire in which lower scores are indicative of greater impairment.
Results
Patients with CFS had far lower mean scores than the general population control subjects on all eight SF-36 scales. They also scored significantly lower than patients in all the disease comparison groups other than depression on virtually all the scales. When compared with patients with depression, they scored significantly lower on all the scales except for scales measuring mental health and role disability due to emotional problems, on which they scored significantly higher.
“PEM or relapse is characteristic. Sleep problems, difficulty with memory or concentration, muscle and joint pain, dizziness, can be accompanied by other co-mobid conditions such as fibro, IBS, TMJ, MCS, etc.
“Key symptoms of the illness definitely interact:
Sleep <--> Pain<--> Fatigue
“Areas of disagreement:
- How long should the duration if fatigue be?
- Number of symptoms required?
- Is PEM required or just one of additional symptoms?
- Which conditions exclude diagnosis (medical/psychiatric illnesses)?
“Highest prevalence in 40-50 year olds, but broad range.”
“More common in women than men three to four fold.”
“Latinos>African Americans>Caucasians
“Most patients ill > 5 years but only 50% of patients seek medical care and only ~16% diagnosed.
“How common is ME/CFS? Pooled prevalence estimate is .31% in the US based on pop-based surveys. Range is .24-2.5% in 3 studies.
“Functional impairment comparable to CHF, MS, cancer, diabets, and lung disease.”
“Consistent finding in multiple studies.
“Showing chart about impairment vs other illnesses AM J Med 101:281-90,1996 by Komaroff. Worth looking at... [see box]
“BBIAB [Be Back In a Bit], this room is “a chemical soup” as my friend here just put it... :roll:
“Someone asked about 1-day vs 2-day exercise tests. They found that ME/CFS patients generally did poorly on 1-day tests so a 2-day test seemed needlessly onerous (not a quote).
“I'm sitting next to Byron Hyde now and am trying to resist telling him how awesome he is 
Daily Fluctuations of Cytokines in ME/CFS Patients

Jarred Younger, MD
Assistant Professor in Pain Medicine
Director of the Adult and Pediatric Pain Lab at Stanford
Searcher 10.55 - 11.20:
“Dr Younger is talking about cytokine fluctuations. Patients have large symptom fluctuations (for example, from 20-80 on a 100 scale.)
“If a patient can get to 80, then it indicates they have the physiological capability to be at 80 all the time. He wants to find the cytokines that explain the difference.
“He tested patients 25 days in a row and had them track their symptoms. He's looked at fibromyalgia patients and ME/CFS.
“As most of us know from the publication, leptin was generally correlated with fatigue.
“Microglia are easily activated when exposed to different stimuli, such as infections, chronic stress. diesel fuel etc.. They also activated more easily with aging. Leptin also lowers threshold for microglia.
“The association with leptin opens up many treatment possibilities. More than Dr Younger could test in his lifetime.
“He listed a lot of meds (such as minocycline, naltrexone) that work on microglia. He also mentioned a lot of herbs (primarily Chinese) that have potential but haven't been studied.”
Gene Expression Findings in ME/CFS
Searcher 11.30 - 12.00:
“Dr. Kaushal is new to ME/CFS and finds it fascinating.
“I don't know what parts of this talk is public so I am going to take notes and confirm it's all public so I can post more info on his talk.”
Lunch and Learn “Media Portrayal of ME/CFS”
Erin Allday
Journalist, SF Chronicle
Natalie Boulton
A Carer, an Artist Activist and Co-Director of the Film “Voices from the Shadows”
David Tuller
UC Berkeley, Department of Journalism
Journalist, SF Chronicle
Natalie Boulton
A Carer, an Artist Activist and Co-Director of the Film “Voices from the Shadows”
David Tuller
UC Berkeley, Department of Journalism
Searcher 12.20 - 13.20:
“They are currently showing a showing a short version of Voices from the Shadows.
“I had not previously seen more than the trailer and it was incredibly moving (and infuriating.)
“I think it was fantastic that they showed the film to a mixed audience that is not all knowledgeable about the potential severity of ME/CFS.
“Phil Bronstein is moderating, and the panel consists of David Tuller, Natalie Boulton (Voices from the Shadows), and Erin All Day (SF Chronicle).
“David Tuller is talking about how much the name affects the coverage of the illness. Everyone has fatigue, and people shorten the illness to "Chronic Fatigue." There's been a lot of effort for the name change.
“Voices from the Shadows is very powerful as is Laura Hilldebrand's piece. Unfortunately only patients and carers seem to have interest in the film, according to the producer Natalie Boulton.
“She talked about why there is no interest in the film-- a lot seems to be the mental health profession's influence on the Science Media Centre.”
“There is a lot of discussion in general about how bad it can be in the UK due to the psychiatric lobby. Simon Wessely comes up often
“It's obviously very hard for people who can't be active to be activists in the same way HIV patients were.
“Once XMRV was out of the picture journalists lost interest.
“There's not an obvious hook, since there are no clear answers, it's not well-defined, and there are not enough clinical studies out there to report on.”
“A lot of attendees are asking questions about Lyme, but it's not a focus from the Stanford side as far as I can tell.
“The idea of Investigative Journalism is coming back (paraphase from Phil Bronstein).”
“Cardiovascular Aging in CFS”
Mehdi Skhiri, MD
Clinical Instructor of Medicine, Associate Medical Director, Night Hospital Medicine Division, Division of General Medical Disciplines, Stanford University Medical Center
Clinical Instructor of Medicine, Associate Medical Director, Night Hospital Medicine Division, Division of General Medical Disciplines, Stanford University Medical Center
Searcher 13.58:
“He first went through the previous cardio studies:
“One showed there was a trend toward reduced LV mass in CFS vs sedentary controls. Reduced stroke content as well. He thinks it's a decent study.
“Second study compared 4 groups: severe CFS, mild CFS, sedentary, and non-sedentary matched on gender and BMI. 15% decreased TBV account for 91-94% of the cavity volume difference. But, he seemed skeptical of some of the study design.
“His study had 3 groups: CFS (25), control: sedentary (26), control: highly active - really high bike score, mainly really active cyclists. (26) MFI-20 for patients: 78.7, for controls: 40.8:
“Overall, patients were similar to sedentary controls on cardiovascular measurements.
No early CV aging or increased CV risks. He doesn't think patients are at any more risk of cardiovascular events than healthy sedentary patients.
He made it clear he couldn't study patients who couldn't exercise at all so he doesn't know how their hearts are.”
“One doctor stood up to say that he had less patients than average develop cardiovascular disease.
“I had participated in this study and spoke with him today. He said there will be more results from the study later in the year.”
MRI Findings in ME/CFS
Searcher 14.56:
“I need to confirm whether these results can be made public as I think they haven't been published yet. If so I will post as soon as I know.
“This session was focused on anatomical brain structure.
Quantitative EEG Studies Suggest Subcortical Pathology in ME/CFS
Marcie Zinn, PhD (pictured)
Research Consultant in Experimental Neuropsychology and Quantitative Electroencephalography, Stanford University Medical Center, Department of Infectious Diseases and Geographic Medicine
Executive Director, Society for Neuroscience and Psychology in the Performing Arts, Performing Arts Psychophysiology Research Institute
Mark Zinn, MM, PC
Director, Attainment Center for Neuroeducation Research Consultant in Cognitive Neuroscience Division of Infectious Diseases and Geographic Medicine Stanford University School of Medicine
Director, Attainment Center for Neuroeducation Research Consultant in Cognitive Neuroscience Division of Infectious Diseases and Geographic Medicine Stanford University School of Medicine
Searcher 17.05 (following permission obtained after presentations):
“I got confirmation from Drs Marcie Zinn and Mark Zinn that I can post their results...
“So far I have found their findings to be the most fascinating of the conference because I am always curious about what is occurring in the brain when we experience "brain fog." I will speak with them more at IACFS/ME.
The following is a summary of Dr. Marcie Zinn's talk:
“They looked at the EEG of patients and controls to see if the Peak Alpha Frequency could help them differentiate patients and controls.
“CFS-patients produced significantly reduced PAF’s (Peak Alpha Frequencies) over 58% of the cortex compared to controls.
“Whenever you see EEGs this widespread there are always cognitive problems and a brain pathology”
“PAF predicted MFI-20 fatigue (lower peak alpha frequency=>higher fatigue scores).
“Implications of these results:
Associated with interruptions in goal-directed behavior:
- reduced ability to coordinate cognitive functions in formation of coherent behavioral sequences.
Parallels mental status change consistent with dysexecutive symptoms (cognitive processing) such as:
- Alertness and Attention
- Memory Performance (WM, STM, LTM— storage and retrieval)
- Temporal organization
- Memory Performance (WM, STM, LTM— storage and retrieval)
- Temporal organization
“EEG can’t be used to diagnose ME/CFS yet but it can be used to evaluate the extent and nature of the brain dysregulation.”
This is a summary of Dr Mark Zinn's talk:
- Many abnormal delta sources in CFS
- Indicates disruptions in short/long-distance information transfer within and across cortical networks
- Deficits in language production
- Many other deficits
- Primary motor deficits
- Sensory ataxia: reduced proprioception
- Disturbances in pain sensations, alterations in processing of sensory stimuli which would lead to hypersensitivity
- Hypo-functioning Broca’s area is consistent with studies showing deficient verbal working memory and language and is consistent with previous findings
- Possible indicator of limbic encephalitis
- Strong evidence of CFS cognitive deficits associated with central fatigue, brain fog in CFS samples without psychiatric co-morbidity
- Increased delta sources in CFS patients may be linked to the a-motivational aspects of fatigue.
Anthony L. Komaroff, MD
The Simcox-Clifford-Higby Professor of Medicine, Harvard Medical School
Senior Physician, Brigham and Women’s Hospital
Searcher 15.30 - 16.10:
“Age: Average Mid-30s. Sex: 65% female (but note that women seek health-care more often than men on average).
“Socioeconomic: Middle-class, but more common among African-American/Latino minority populations on population-based surveys.
“Education: 50% college grads in office-based samples.
“Severity: 50% intermittently bedridden. 81% of his patients get increased fatigue after physical exertion.”
“Only common physical examination abnormality was posterior cervical adenopathy at 35%-45% and impaired serial 7's at 30-40%
“He showed the same chart from the 1996 study I earlier mentioned which indicated that CFS patients had worse functioning than any other group he studied.
Dr Komaroff's summary:
Evidence of CNS Involvement in CFS:
- Neurodendocrine dysfunction
- Information processing impairments not explained by concomitant psychiatric diseases
- Autonomic dysfunction
- MRI Findings
- Areas of reduced signal in Spect
- Increased lactate in CSF
“Dr Komaroff thinks the evidence shows that something has activated several different parts of the immune system. What has activated it is unclear. He walked through the many potential infectious agents linked to CFS.”
“Great comment from an audience member (a Phoenix Rising member) about CBT:
- The studies on it have been done on Oxford and not Fukuda.
- CBT isn't usually used for coping with disease, instead it's used to convince patients they don't have an illness.
- When we do objective studies, people don't increase activity after CBT even if they self-report improvement.
“If the organism experiences a lack of energy, perhaps there is a defect in energy metabolism at the cellular level.”
Dr. Komaroff's current view:
“...could the symptoms of CFS result from a chronic low-grade encephalitis?”
“He's finishing by going through treatments. It's the standard list of sleep meds, CBT to deal with symptoms, GET very carefully done.
“But he has been careful to note throughout the presentation that this an expression of somatic symptoms by people with physiological disorder.
“There is extensive research to show differences between patients and controls.
“An audience member asked about TMS. He hasn't tried it and doesn't know of any studies on it. He thinks anecdotally 50% of patients have some response, but he doesn't know of anyone who had a strong response.
“Dr Komaroff answered another question by saying 10-15% of his patients fully recover although some relapse. He hasn't found anything that can predict who will recover.
“Circulating Cytokines in ME/CFS Patients Reveal a Novel Inflammatory and Autoimmune Profile”
Jose G. Montoya, MD, FACP, FIDSA
Professor of Medicine, Division of Infectious Diseases and Geographic Medicine Stanford University School of Medicine
Director, Palo Alto Medical Foundation Toxoplasma Serology Laboratory
Searcher 17.10:
“Dr Montoya's talk. With much thanks to a fellow patient, Epiphany, for assistance and note-taking
“The following relates to his latest study:
“1. They measured 51 cytokines at the same time, 2 serums taken 2/day to control for variations
“2. Two-sided independent t-test, linear regression, linear regression, LASSO method
“3. Cytokines are a highly interconnected network, so very complicated
“4. Healthy control cases (similar ages, gender distribution, PEM was present in 96% of patients who met the Fukada criteria):
- 26 cytokines decreased over time, associated with age
- important because we need to control for age
- cytokine differences between females (Leptin, ENA78, IL1RA, Resistin are all higher) v. males
- certain cytokines were higher in CFS v. control (abnormal, proinflammatory)
1. Healthy patients v. Sick: less cytokines
- theory: mild shift of cytokines from blood to tissue containing inflammation; as inflammation progresses in tissues, then cytokines spill over back to blood:
- other theory: initial stages - down regulation in the acute phase
2. Toxoplasmosis: patients dump cytokines during early stage of infection (immune system reduce cytokines in peripheral blood)
“6. 13 cytokines related (these were identified as increasing with CFS severity): related to the following responses: cell trafficking, cell activation, cell growth and differentiation, cytokine production, Th1 v. Th2 responses
“7. IL-17 = cytokine associated with autoimmune disease (RA, IBD, MS); 2 cytokines are also highly associated with females
“8. Patients are more likely to have illness for longer with lower TGF-B levels (a powerful anti-inflammatory cytokine)!
- As disease lasts longer, the immune system loses its capacity to suppress inflammatory T cell responses
- progressive increase of cytokines+ decrease of anti-inflammatory cytokine with disease duration
- PATIENTS: BODIES INFLAMED, SENSITIVITY TO STIMULI, PAIN --> supported!
- 12 cytokines identified as having a dose response behavior
- IL 17- autoimmune side
- data opens door for treatment with anti-inflammatory agents to treat other inflammatory diseases
“There is a great deal of momentum in determining the pathogenesis of CFS
“There is an accepted urgency in CFS research and clinical treatment now
“The number of people in attendance here today is a testament to that urgent need.
Microbial Diagnostics and Discovery in ME/CFS

W. Ian Lipkin, MD
John Snow Professor of Epidemiology and Director Center for Infection and Immunity Mailman School of Public Health
Professor of Pathology and Neurology College of Physicians & Surgeons Columbia University
Searcher 17.25:
“Most diseases have origins in animals, not humans.
“Most important person in identifying a pathogen is the clinician, not the laboratory.
“He is showing a slide called "Models for Bacterium-triggered mental illness: CNS autoantibodies in mice exposed to group A Steptococci"
“The slide shows a video of a mouse doing compulsive behaviors. The researchers can see the antibodies in the mouse brains after autopsy which can also be seen in humans.
“Toxins can also lead to antibodies.
“Their hypothesis is that Kawasaki's disease is caused by an autoimmune reaction to candida in the troposphere.
“25% of autistic children have GI complaints. Researchers looked at GI tract and found that some enzymes were low in breaking down complex sugars.
“This may explain why some children are helped by antibiotics or dietary restrictions.
“The children were also low in certain enzymes that break down toxins.
“These enzymes are critical for breaking down xenobiotics.
“HIV patients who don't respond well to anti-retrovirals have high cytokines in reaction to pathogens. Prevotella seems like a key culprit and may need to be treated
“They have also discovered new viruses that are in ticks.
“Chronic Fatigue Initiative Plasma Study (recent study as reported in 'Lipkin finds biomarkers not bugs', last year):
- 265 CFI serum samples (215 patients, 50 controls)
- 2 cases of HHV6.
- In 586 plasma samples they found HHV-6 in 6 samples (4 cases, 3 controls), HHV-6B in 3 cases, 1 control.
- Generally HHV-6 has been the same in cases and controls.
- Retroviruses were found in ~85% of 285 samples. Equivalent in cases and controls. Annelloviruses were found in ~75% of sample pools, and was similar in cases and controls.
“They would like to do microbiome tests on the CFS samples. They are waiting on funding. IRB is in progress.
“Dr Lipkin doesn't think it's feasible to do many tissue biopsies since we should see antibodies to the viruses (e.g. enteroviruses) if they are present in the blood analysis.
“The number of bacteria in the body outnumber human cells 10 to 1. Hundreds of people studying the microbiome have learned that the bacteria in our digestive system are not inert.
“He thinks the microbiome is the area that makes the most sense to focus on. It's hard to get funding. He said one paper reviewer mentioned psychogenic illness in regards to ME/CFS so he had to look elsewhere.
[Note: Read the recent Interview with Dr. Lipkin and his public appeal for a ME/CFS Microbiome Study.]
“Dr Fletcher said they have a grant to study microbrial translocation in ME/CFS. They will look at 4 timepoints over 18 months.
The End.
Searcher, summing up...
“I can't write much of a summary because I am super-fried but here's a short one:
“There were hundreds of attendees. They needed to move us to a bigger room because the regular room was standing-room only. I met a lot of patients, researchers, ME/CFS focused clinicians, and general physicians who see ME/CFS patients on occasion.
“The conference was super-intense. There were few breaks and even lunch had the Voices from the Shadows screening and the journalism talk.
“They had a lot of information to fit in one day, which is a great sign that Stanford is doing a wide-range of research with potential impact.
“I think there was a palpable sense that progress is finally being made. Most of the research shows significant differences between patients and controls. Some of the research (like Younger's) point to treatment options that are worth testing.
“There is, not surprisingly, frustration that there is not more funding to do research.
“Many of the who's who of ME/CFS research seemed to be there. In no particular order and not including everyone, I saw Dr Montoya, Dr Kogelnik, Dr Byron Hyde, Dr Peterson, Dr Klimas, Dr Fletcher,Dr Vernon,Dr Komaroff,Dr Friedberg, Anne Whittemore, Carol Head (head of CAA).
“There is some overlap with IACFS/ME (like Lipkin and the Zinns) so we should have additional info then.”
Phoenix Rising is a registered 501 c.(3) non profit. We support ME/CFS and NEID patients through rigorous reporting, reliable information, effective advocacy and the provision of online services which empower patients and help them to cope with their isolation.
There are many ways you can help Phoenix Rising to continue its work. If you feel able to offer your time and talent, we could really use some more authors, proof-readers, fundraisers, technicians etc. We’d also love to expand our Board of Directors. So, if you think you can help in any way then please contact Mark through the Forums.
And don’t forget: you can always support our efforts at no cost to yourself as you shop online! To find out more, visit Phoenix Rising’s Donate page by clicking the button below.
View the Post on the Blog
Last edited by a moderator: