Scandinavian neuropsychopharmacology
Michael Sharpe has his name on this Schrder, Fink et al paper
PDF: http://scnp.dk/journal/index.php/SCNP/article/viewFile/105/5
SCANDINAVIAN NEUROPSYCHOPHARMACOLOGY
2010 VOL 3
Page 13
The STreSS-1 trial: an example of a novel unified treatment approach for functional somatic syndromes
Andreas Schrder, Emma Rehfeld, Eva rnb, Michael Sharpe, Ramus W. Licht, Per Fink
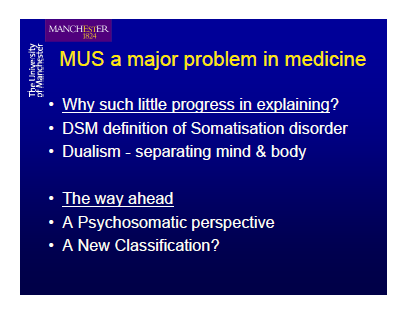
Treatments based on active patient involvement like exercise and cognitive behavioural therapy have proven effective in various functional somatic syndromes (FSS) such as fibromyalgia and irritable bowel syndrome. However, the delivery of such treatments is problematic. This is because FSS are typically managed in secondary care medical services which are organised into disease-focussed medical specialties. Recently, bodily distress syndrome was introduced as a unifying diagnostic category that covers most FSS etc
The Research Clinic for Functional Disorders and Psychosomatics, Aarhus University Hospital, Denmark, The Research Clinic for Functional Disorders and Psychosomatics Aarhus University Hospital Noerrebrogade 44 8000 Aarhus C, Denmark
andreas.schroeder@aarhus.rm.dk
---------------
and from 2007:
PDF:http://www.urotoday.com/index2.php?option=com_content&do_pdf=1&id=2205779
Symptoms and Syndromes of Bodily Distress: An Exploratory Study of 978 Internal Medical, Neurological, and Primary Care Patients
Contributed by Philip M. Hanno, MD
Wednesday, 02 May 2007
BERKELEY, CA (UroToday.com) - The introduction of this fascinating exploratory study of almost 1000 internal medical,
neurological, and primary care patients states the following: "Medically unexplained or functional somatic symptoms are
complaints defying the clinical picture of known, verifiable, conventionally defined diseases and unbacked by clinical or
paraclinical findings.
They are prevalent in all medical settings and may be persistent, disabling, and costly." Specifically, Fink and colleagues
from Denmark are referring to chronic fatigue syndrome, fibromyalgia, irritable bowel syndrome, chronic benign pain
syndrome, and other somatoform disorders. One cannot help but notice that many of these syndromes have been
associated with bladder pain syndrome (PBS/IC).
In this study, the 978 patients consecutively admitted from a neurological department, a medical department, and from
one primary care were interviewed using the Schedules for Clinical Assessment in Neuropsychiatry diagnostic instrument
(SCAN). Patients complained of a median of 5 functional somatic symptoms. No single symptoms stood out as
distinctive for patients with multiple symptoms. Principal component factor analysis identified a cardiopulmonary
including autonomic, a musculoskeletal, and a gastrointestinal symptom group explaining 36.9% of the variance. Latent
class analysis showed that the symptom groups are likely to materialize in the same patients, suggesting that they are
different manifestations of a common latent phenomenon.
Latent class analysis using inclusion of a group of 5 additional general unspecific symptoms allowed construction of
clinical diagnostic criteria for "bodily distress disorder." Patients were divided into nonbodily distress (589), modest bodily
distress (329) and severe bodily distress (60). The latter categories had a prevalence of 25% and 3% respectively.
The authors believe their data supports previous findings that the existence of specific functional somatic syndromes is
an artifact of medical specialization. They identified a general, distinct, bodily distress syndrome or disorder
encompassing the various functional syndromes advanced by medical specialties as well as somatization disorder and
related diagnoses of the psychiatric classification. The syndrome can manifest as gastrointestinal, cardiopulmonary, or
musculoskeletal problems.
While in no way referring to painful bladder/interstitial cystitis, the authors have taken a novel way of looking at a variety
of syndromes often seen to accompany PBS/IC. Many are looking for a new paradigm within which to place the myriad
of symptoms and problems associated with painful bladder patients, and this is seemingly a start.
Per Fink, Tomas Toft, Morten Steen Hansen, Eva rnbl, and Frede Olesen
Psychosomatic Medicine, 69(1):30-39, 2007
UroToday.com Painful Bladder Syndrome Section