Part 3: The Missing Voices Speak Up in Mexico
In the last of a three-part series, people with neuroimmune diseases in Mexico speak up about the wide-ranging consequences of the disease on their life. If you haven’t already read the first part of this series, click here.
By Eric Pyrrhus
"There's so many mysterious or surprising variables in chronic illness," comments 35-year-old María Richardson, originally from Monterrey.
"At home I can move around the house, but I need to be mindful of pacing my activities, since my heart rate rises considerably when I am standing. But commuting to work is not possible for me at present. Neither is having a full work schedule, at the pace at which most people can work."

Even when María Richardson is trying to stand up for her rights, her disease forces her to remain seated.
Image courtesy of Millions Missing México.
María suffers from myalgic encephalomyelitis/ chronic fatigue syndrome (ME/CFS) and postural orthostatic tachycardia syndrome (POTS), which means that she is forced to spend much of her time lying down, with debilitating weakness and cognitive dysfunction.
Her disease is very hard for her, especially because she has spent her life as a very active person — dancing ballet, flamenco, and other complex styles since she was only two years old.
"It seems surreal to me now that I used to walk to work, step right into action, and be able to walk back home. And I used to shower standing up every day!"
Multiple doctors dismissed her symptoms and even mocked her. "I had some really hurtful interactions earlier in my quest for a diagnosis," she relates.
"Doctors describe both ME/CFS and fibromyalgia as conditions that are related mostly to emotional wellness, citing stress reduction and exercise as treatment. They really buy into the narrative of women being more emotional and therefore more psycho-somatizing, and ultimately have little to offer patients."

After years of mistreatment by doctors, Carmen Cuevas was left with even more problems and even more diagnoses. Image courtesy of Carmen Cuevas.
Some patients have been treated even worse by doctors.
"I have been treated for years as a psychiatric patient at the public hospital in Morelos and at the López Mateos Hospital in Mexico City," explains historian Carmen Cuevas, from Morelos, in a 2021 interview.
"In a checkup, a neurologist told me that the involuntary movements I had were due to unresolved psychological problems and that I was faking everything. After insisting, they sent me for clinical studies and I was diagnosed with dystonia and severe dysphonia (which was caused by their medication!)"
Carmen suffers from fibromyalgia, ME/CFS, and myasthenia gravis. But she says that her medical treatment only resulted in even more problems and even more diagnoses.
"I had to criminally sue several doctors for the irreversible damage caused. Curiously, the psychiatrist always defended me by saying that I did not have a mental problem and told me that if they said I was crazy, they had to prove it."
Unfortunately she lost her lawsuit, leaving her devastated. "My working life and salary were destroyed, after being a post-graduate historian with a good salary — and my disability pension is miserable."

Elizabeth Macías has valiantly tried to live a normal life after falling ill with fibromyalgia at only 15 years old. Image courtesy of Elizabeth Macías.
"There's the problem that many doctors don't believe in the condition and think you're just faking it," explains 27 year-old Elizabeth Macías from Aguascalientes, who runs a popular website for patients.
"One doctor told me 'don't come to me with these inventions, you don't have anything!'"
Elizabeth Macías has suffered with fibromyalgia since she fell ill at only 15 years old. But she has valiantly strived to live a normal life.
"When I got sick I had to drop out of school, and a year later I managed to re-enter high school. With a lot of effort, help from teachers and coming home crying every day for having to endure the pain, fatigue and cognitive problems, I managed to finish high school."
"I have tried to work but I had to give it up because there comes a point where my body simply doesn't respond. I even only made it through one day. Every time I went through this, where I had to give up what I was doing, it had a very strong impact on me."
"I still have a lot of frustration because no matter how hard I fight, I just can't do what I want to do — no matter how hard I work on my health, I always end up having crashes and getting worse."
"I try to exercise as much as I can, but even if I do a little — I have a limit, and if I exceed it the crash comes. Sometimes it comes that same day or the next day. The same happens with the day-to-day activities I do — if I go over the limit my body can take, it triggers a crash."
Exercise: helpful or hurtful?
In modern years, doctors have tried to improve the symptoms of various diseases by encouraging patients to exercise. In some conditions, such as cardiovascular fatigue or rheumatological joint pain, this advice has proven to be a great benefit to patients.
Some doctors have become so encouraged by such findings that they suggest that all diseases would benefit from exercise. But every rule has its exceptions. And neuroimmune diseases are very different from cardiovascular fatigue or rheumatological joint pain.
Thirty years ago, doctors were trying to define ME/CFS based on the single symptom of fatigue and doctors were trying to define fibromyalgia based on the single symptom of pain. Both over-simplistic approaches failed. Many people who only had chronic fatigue were incorrectly diagnosed with ME/CFS and many people who only had chronic pain were incorrectly diagnosed with fibromyalgia.
Some old clinical studies that relied on these outdated definitions reported positive results for the use of exercise to improve symptoms.
Other researchers questioned these old studies, stating that "study results are varied and do not provide a uniform consensus that exercise is beneficial [in fibromyalgia]" and that "there is still no evidence of any long-term treatment-related benefits [of exercise in ME/CFS]."
The details of this physiological process are still not entirely clear, but researchers are currently trying to understand it better.
A systematic review of the research, which focused on the symptom of pain, found that "compared with healthy controls, aerobic exercise significantly increased pain severity" in patients with ME/CFS or fibromyalgia.
In addition, "increases in clinical pain between 8 and 72 hours after exercise were greater than those [immediately] after exercise."
______________________________________________________________________________________

________________________________________________________________________________________
A systematic review of studies by the Cochrane Collaboration concluded that there is "little scientific evidence" for the effectiveness of exercise in fibromyalgia.

________________________________________________________________________________________
A systematic review of studies by the Cochrane Collaboration concluded that there is "little scientific evidence" for the effectiveness of exercise in fibromyalgia.
But what about exercise in patients who are correctly diagnosed according to the modern diagnostic criteria for ME/CFS or the modern diagnostic criteria for fibromyalgia?
The modern diagnostic criteria for ME/CFS, put together by an international committee of experts, says that the defining characteristic of ME/CFS is post-exertional malaise (PEM), also known as post-exertional symptom exacerbation (PESE), which is a significant and abnormally prolonged worsening of symptoms in response to exertion.
This means that any exertion, including exercise, triggers a physiological process that eventually results in a significant worsening of all symptoms, typically appearing one to two days after the exertion.
Although patients often do not experience a change in symptoms immediately after the exertion, and may even feel slightly better immediately after the exertion, the situation worsens dramatically — and sometimes suddenly — one to two days after the exertion.
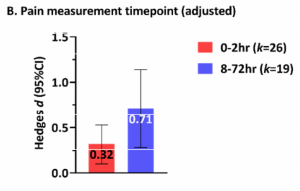
A review of the research found that pain significantly increased in patients with ME/CFS or fibromyalgia 8-72 hours after exercise.
Image is supplemental figure 4B from Barhorst et al., Pain-Related Post-Exertional Malaise in Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia: A Systematic Review and Three-Level Meta-Analysis, Pain Medicine, Volume 23, Issue 6, June 2022.
Public domain.
But what about the effects of long-term, gradual exercise training, as opposed to just a single episode of exercise? Could long-term, gradual exercise training overcome any negative effects of the post-exertional symptom exacerbation?
In 2019, the health authority of the English government commisioned a survey of ME/CFS patients to find out the effects of long-term, gradual exercise training. According to the results of this research, 67-75% of patients who had tried long-term, gradual exercise training reported that they had suffered a long-term deterioration in their physical health.
Many patients had suffered such a significant deterioration in their physical health that they were no longer able to leave their bed.
As a result, in 2021, the health authority of the English government issued formal recommendations to doctors that explicitly warned "do not offer people with ME/CFS any program that uses fixed incremental increases in physical activity or exercise."
Both genders suffer
"The Mexican government labels fibromyalgia as a women's disease, since 'we are more prone to the stress of daily life,'" explains Daniela Herrera Villarreal, originally from Oaxaca. "In Mexico we have a big problem of gender bias in medical services, as these are the ideas that prevail."
"I was constantly harassed by neurologists with questions about my personal life — especially if I was okay with my partner, if I got along with my dad, if I had sexual desire and other very sexist questions," she explains further. "Many women have contacted me telling me similar stories or much worse."
"I remember an alternative therapist who concluded that I suffered from 'blocked libido' and was offended when I didn't accept his sex therapy," recounted María Richardson in a 2017 article.

A viral internet meme reminds people that "men suffer from fibromyalgia, too."
"One doctor told me he didn't think I had ME/CFS because, according to him, it's a disease that occurs mainly in women," recalls Yoshiro, a 35-year-old man from Mexico City.
"Obviously that doesn't mean it can't occur in men, so I was left with the impression that he used a fallacious argument to keep me from insisting on the diagnosis."
Yoshiro suffers from a severe form of ME/CFS that leaves him almost entirely confined to his bed.
"I spend about 22 hours in bed a day, although I can stand at times to go to the bathroom and eat. I have recurring headaches, sensitivity to light and various other symptoms that I have to deal with on a daily basis."
"I studied English literature, but the brain fog made it impossible for me to finish my thesis and get my degree. I also used to do freelance translations, but similarly I had to stop working because of exhaustion and cognitive difficulties."
Like most patients, he encountered much disbelief from doctors.
"It took years for my parents, who are doctors, to take my illness seriously. (I was told the classic phrases 'pull yourself together', 'it's just a question of attitude', etc.) A neurologist I went to for consultation saw that my test results were normal, and told me that there was definitely nothing physically wrong with me and that I had probably suffered psychological trauma."
"It is not clear to me if my experience has been very different from that of women with ME/CFS in Mexico. I definitely haven't found the medical support I would have liked to have had, but perhaps, being a man, it's harder for them to chalk my symptoms up to hysteria or some equivalent."

Carlos Alberto fell ill with fibromyalgia and ME/CFS in university.
Image courtesy of Carlos Alberto.
Carlos Alberto is a 34-year-old lawyer who fell ill with fibromyalgia and ME/CFS 12 years ago, in his last year of university.
"From the moment I open my eyes, I have already had nightmares — or uncomfortable dreams — where I have been looking for the cure," he relates. "What comes next may depend on the weather, medications, or what needs to be done that day.
"If you are alone, well, it's up to you if you suffer an attack or endure the one you already have. There are some attacks of fatigue that completely prevent you from moving. It's as if they drain away all your energy. Another type is when the pain skyrockets.
"Exercise means being in bed for three to five days afterwards, and while you're doing that the pain is unbearable," he explains. "It's like sticking your hand in the fire. Okay, you can do that, but after once or twice — do you really want to do it again?"
Carlos finds it especially hard that few people seem to understand the disease. "Sometimes you're better than other days. Then you hear 'why don't you just do every day like what you do today?' Everyone judges."
Fortunately, he has found support from his online community. "The treatment that allows me to function, I did not find it in Mexico — but by talking to other patients world-wide. When what they say mirrors exactly how you feel, even online, you realize that you are not crazy and that maybe you can live with it after all."
When the stigma turns violent
Carlos Gil, a 32-year-old engineer from Mexico City, had to give up his career as an engineer because of the overwhelming cognitive dysfunction that came with his fibromyalgia. "My body is slowly shutting down and there's nothing I can do to stop it," he said.
On a fictional television show, his brothers had heard a doctor say that fibromyalgia wasn't a real disease, rather just an excuse for people who are too lazy to work. This idea stuck in their heads, and as a result his family kicked him out of the house, leaving him homeless.
"Incomprehension, mistreatment, humiliation, oblivion, is the condemnation for the fibromyalgia patient. We are destined to banishment and abandonment, to disrepute," he concluded.
He ended up working as a security guard in a market, a job he took advantage of to have a roof over his head and to rest from the overwhelming fatigue. When his shift was over, he would wander the streets or lie down on a park bench. He had only his girlfriend Alicia, who wanted to help him and provide for him.
And yet, his brothers would not leave him alone. Having heard that fibromyalgia was a "woman's disease," they attacked him, saying that all he needed now was to get cervical cancer or menopause.
Desperate, Carlos contacted a prominent patient advocate, Verónnica Scutia.
"I gave a press conference and talked about how there were men who were harassed by their families for suffering from women's diseases," says Verónnica.
"At the press conference, when I was asked how many women patients there were for every male patient, I told the case of Carlos. I mentioned that the violence and discrimination could be worse than in the case of a woman, because in a patriarchal and macho society the man must be strong, and first and foremost a provider."
The next day an article appeared in a major Mexican newspaper, quoting Verónnica's press conference.
Verónnica was thrilled that the article mentioned how patients can suffer from violence and discrimination as a result of their illness.
"Finally they are beginning to talk about how we are victims of VIOLENCE and DISCRIMINATION; in addition to the fact that we can be mistreated as mentally ill," she wrote on her Facebook page.
However, the short article mentioned nothing about male patients or about Carlos's story. Instead, it misquoted Verónnica with a most unfortunate statement: "It is a gender disease, as nine women for every man have it."
Soon after Verónnica posted the article to her Facebook page, she was contacted by Carlos. He had seen the article and was clearly worried. "While before they judged me and assaulted me because of their simple and ignorant ideas, now they have 'justification'," he wrote.
A few hours later, Verónnica received a message from Carlos's girlfriend Alicia. "I was walking with my boyfriend today. It had been so long since we had gone out and I had a hard time getting him to trust me and let me take care of him," she wrote.
"Suddenly six guys came up to us (his brothers with some friends). They brought a stone wrapped in the newspaper article, which they threw at my boyfriend's face. They pushed me and groped me in front of him while they beat him [with shouts of] 'GENDER DISEASE'."
"They beat him horribly, tore his clothes and exhibited him simulating a sexual act, because 'at the end of the day he wants to look like women', and because they 'have always known he is a fa*got and that's what he likes'," she continued.
After this brutal act Carlos and Alicia went to Alicia's house. While Alicia was changing, Carlos took the opportunity to slip out the door.
"Right now I don't know where he is," a concerned Alicia told Verónnica.
"I can't find him and it worries me, because I finally got him to leave his job, to live with me, and now there is nowhere else for him to go. I'm afraid he will do something horrible, but I have nothing left to do but wait, I don't know where to go, where to look for him, he left his cell phone in the apartment ..."
The rest of the day, people waited anxiously for Carlos to return or to communicate in some way. The husband of one patient, who worked for the Red Cross, went out to look for him.
The next day, at 2 p.m., Verónnica received a brief message from Alicia. "He has just shown up. I just now want to forget all this, and he ... he ... I don't want to say it, he will not live with this anymore, thank you and goodbye," wrote Alicia.
Around the same time, a black ribbon appeared on Carlos's Facebook profile.
"We didn't find out what happened. Whether Carlos committed suicide or died as a consequence of the beating," wrote Verónnica in an article eight days later. "Oh, the irony of fate."
Oh, the irony of fate
What happened to Carlos Gil affected Verónnica Scutia greatly.
For years, Verónnica had tried to raise the issue of violence in the patient community, but few people wanted to talk about it. She had even collaborated with a university researcher to conduct a survey of patients, asking about various types of harassment or violence that they may have suffered.
But Verónnica herself had no problem talking about it.

In 2018 Verónnica Scutia shared photos of bruises from a beating that she endured.
Image courtesy of Verónnica Scutia.
In a 2013 article she described how she had lost the sight in one of her eyes due to a beating she had sustained.
"Last November I was beaten, which caused a detachment of my retina. The people around me justify the beating as I am 'a burden and a lazy person who doesn't work or do anything and makes everything up'."
In a 2016 article she described the effect of the violence on her barely nine-year-old son.
"My son also pays the consequences: he lives in terror. To such a degree that he confessed to me that when there is yelling and fighting — which is a habit — he wants to throw himself off the second-floor balcony."
In fact, in the last year alone, she has suffered at least three major attacks.
On August 30, 2021 she related "again they beat me 'because everyone says I'm crazy, and I'm a burden.' They also threw two crystal glasses at me. I also found out today that they told my brother to kick my son and me out of the house because he is my responsibility and that fibromyalgia is a 'disease of lazy, dirty, kept old women'."
On December 21, 2021 she recorded a video of the aftermath of an attack:

A few days before Christmas in 2021, Verónnica Scutia recorded the aftermath of an attack.
Video courtesy of Verónnica Scutia.
Verónnica believes that abuse in the patient community is more common than people would like to admit.
"Domestic abuse is common among the patient community. Some experience psychological abuse, they are not spoken to, they are ignored by the family; others are not given food; others have been stripped of all their possessions; and there are others who have been thrown out of their homes."
Hope springs eternal
For all the tragedy that patients have endured, the future may bring hope.
As more patients speak up and connect with each other over the internet, they become more empowered. As more patients become empowered and people around them learn the truth, old stereotypes break down.
As old stereotypes break down, doctors are forced to confront the truth and re-evaluate what they had been taught.
Progress is slow, sometimes painfully slow, but as more people learn the truth about neuroimmune diseases, the future for patients looks just a little bit brighter.
Learn more!
If you found this series informative, take a look at the following interview about the reality of living with Long COVID in Mexico:
Long COVID in Mexico:
Isolation and Disbelief

In Mexico, patients with Long COVID are shocked by the new reality they face.
Photo courtesy of César Medina.
________________________________________________________________________________________
Isolation and Disbelief

In Mexico, patients with Long COVID are shocked by the new reality they face.
Photo courtesy of César Medina.
________________________________________________________________________________________
Eric Pyrrhus is a scientist with an interest in flaviviruses, picornaviruses, and imaging technology. With undergraduate training at Columbia University and the University of Pennsylvania, and graduate training at U.C. Berkeley and UCSF Medical School, he has studied biomedical sciences, bioinformatics, biomedical imaging, biosensors, computer science, artificial intelligence, and business administration.
Last edited:

