Free full text at: http://bmjopen.bmj.com/content/4/11/e005798.long
For anyone interested, one can also read the review history here: http://bmjopen.bmj.com/content/4/11/e005798.reviewer-comments.pdf and the earlier drafts here: http://bmjopen.bmj.com/content/4/11/e005798.draft-revisions.pdf
For anyone interested, one can also read the review history here: http://bmjopen.bmj.com/content/4/11/e005798.reviewer-comments.pdf and the earlier drafts here: http://bmjopen.bmj.com/content/4/11/e005798.draft-revisions.pdf
BMJ Open 2014;4:e005798 doi:10.1136/bmjopen-2014-005798
Longitudinal follow-up of employment status in patients with chronic fatigue syndrome after mononucleosis
- Health economics
+Author Affiliations
Abstract
- Received 28 May 2014
- Revised 31 October 2014
- Accepted 6 November 2014
- Published 26 November 2014
Objective To examine the effect of early clinical and demographic factors on occupational outcome, return to work or awarded permanent disability pension in young patients with chronic fatigue syndrome (CFS).
Design Longitudinal cohort study.
Intervention A written self-management programme including a description of active coping strategies for daily life was provided.
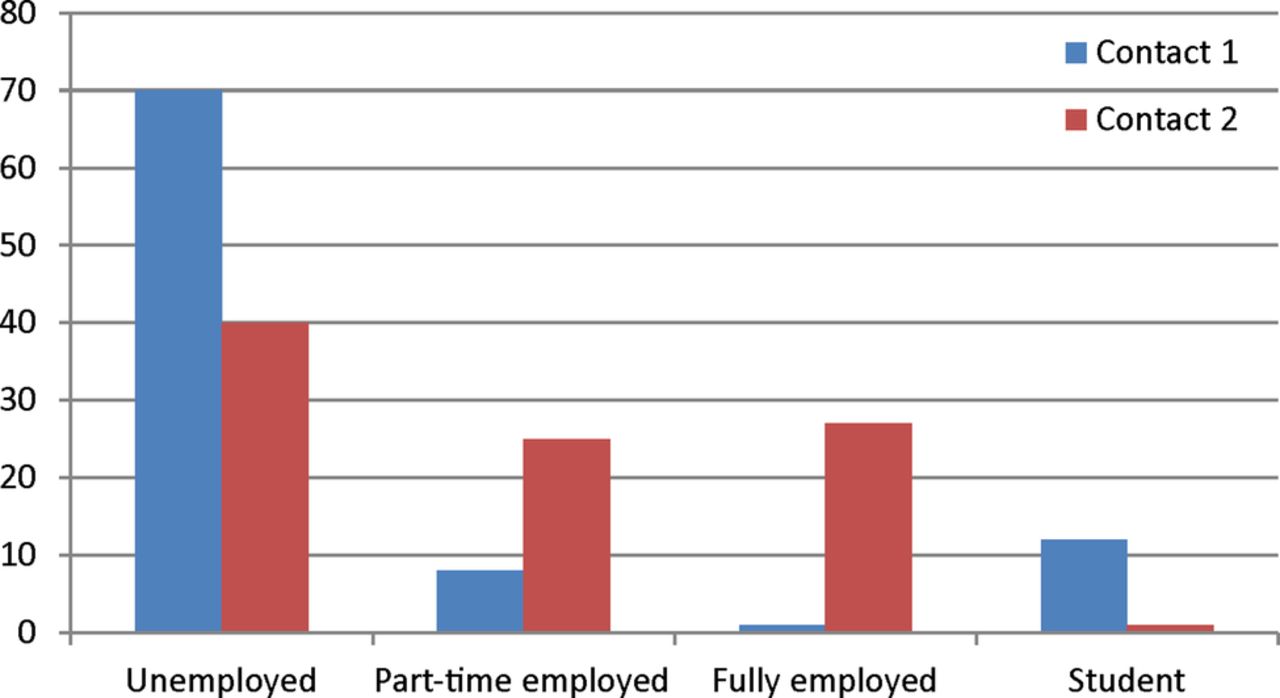
Setting, participants Patients with CFS after mononucleosis were evaluated at Department of Neurology, Haukeland University Hospital during 1996–2006 (contact 1). In 2009 self-report questionnaires were sent to all patients (contact 2).
Primary and secondary outcome measures Primary measure was employment status at contact 2. Secondary measures included clinical symptoms, and Fatigue Severity Scale (FSS) scores on both contacts, and Work and Social Adjustment Scale (WSAS) at contact 2.
Results Of 111 patients at contact 1, 92 (83%) patients returned the questionnaire at contact 2. Mean disease duration at contact 1 was 4.7 years and at contact 2 11.4 years. At contact 1, 9 (10%) were part-time or full-time employed. At contact 2, 49 (55%) were part-time or full-time employed. Logical regression analysis showed that FSS≥5 at contact 2 was associated with depression, arthralgia and long disease duration (all at contact 1).
Conclusions About half of younger patients with CFS with long-term incapacity for work experienced marked improvement including full-time or part-time employment showing better outcomes than expected. Risk factors for transition to permanent disability were depression, arthralgia and disease duration.
Strengths and limitations of this study
- Two strengths of the study are very long prospective follow-up period and focus on employment.
- A limitation is that patients were recruited from a tertiary centre.
- Long-term prognosis for young patients with chronic fatigue syndrome after mononucleosis is favourable for a large subgroup.
- More than half of the patients with long-term incapacity for work are re-employed after mean disease duration of 11.4 years.
- Factors associated with poor long-term prognosis include depression, arthralgia and disease duration.