Hi everyone,
I thought I'd start a log detailing my treatment with MCAS and Primary Immunodeficiency (antibody deficiency).
But before that here's the theme to this log: Life to Fix by The Record Company
Here is my intro post detailing my experiences, symptoms and battle plan with MCAS: https://forums.phoenixrising.me/ind...iciency-mthfr-opportunistic-infections.61324/
Right now, am on daily Hydroxychloroquine, oral albuterol and aspirin (did aspirin desensitization). I'm also on monthly Xolair for the past 10 months. I also cycle through 6 different corticosteroids every 5-8 days, as I develop intolerances to them pretty quickly but with Xolair I'm able to at least partially reset some of the intolerance. I'm allergic to all these drugs, including Xolair, but with the right balance and timing they each help at least a little.
I'm about to do my 4th IVIG infusion this week. Doc is increasing dosage slowly, was on 25g and will be doing 27g now. I have yet to see any benefit from the IVIG for my MCAS. We will be slowly increasing the dosage with each month in the hopes that a higher dose will eventually help with the MCAS. Was prescribed this primarily for my Primary Immunodeficiency, though I still did develop a finger infection just recently but is all better now.
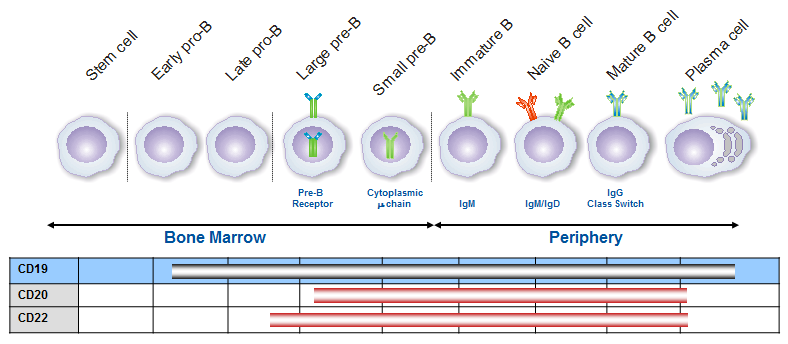
I've also started Rituxan, as prescribed by my Hematologist after consulting with my Immunologist. Had my 1st Rituxan infusion of 1000 mg almost 2 weeks ago. Next infusion is tomorrow. So far, no changes in symptoms, was informed it takes at the very least 2-4 weeks to see a difference. Here's thread detailing some more information about my experience about getting it prescribed and lots more good info: https://forums.phoenixrising.me/index.php?threads/how-to-get-prescribed-rituxan.61530/
If anyone has anything they want to add (advice, opinions, studies, anything) I'd be more than happy if you did. I see tremendous benefit in gathering the thoughts and opinions of others in addition to the massive amounts of research done on one’s own. Any questions are also welcome. Hopefully this also proves useful to others with MCAS.
Cheers for the best!
I thought I'd start a log detailing my treatment with MCAS and Primary Immunodeficiency (antibody deficiency).
But before that here's the theme to this log: Life to Fix by The Record Company
Here is my intro post detailing my experiences, symptoms and battle plan with MCAS: https://forums.phoenixrising.me/ind...iciency-mthfr-opportunistic-infections.61324/
Right now, am on daily Hydroxychloroquine, oral albuterol and aspirin (did aspirin desensitization). I'm also on monthly Xolair for the past 10 months. I also cycle through 6 different corticosteroids every 5-8 days, as I develop intolerances to them pretty quickly but with Xolair I'm able to at least partially reset some of the intolerance. I'm allergic to all these drugs, including Xolair, but with the right balance and timing they each help at least a little.
I'm about to do my 4th IVIG infusion this week. Doc is increasing dosage slowly, was on 25g and will be doing 27g now. I have yet to see any benefit from the IVIG for my MCAS. We will be slowly increasing the dosage with each month in the hopes that a higher dose will eventually help with the MCAS. Was prescribed this primarily for my Primary Immunodeficiency, though I still did develop a finger infection just recently but is all better now.
I've also started Rituxan, as prescribed by my Hematologist after consulting with my Immunologist. Had my 1st Rituxan infusion of 1000 mg almost 2 weeks ago. Next infusion is tomorrow. So far, no changes in symptoms, was informed it takes at the very least 2-4 weeks to see a difference. Here's thread detailing some more information about my experience about getting it prescribed and lots more good info: https://forums.phoenixrising.me/index.php?threads/how-to-get-prescribed-rituxan.61530/
If anyone has anything they want to add (advice, opinions, studies, anything) I'd be more than happy if you did. I see tremendous benefit in gathering the thoughts and opinions of others in addition to the massive amounts of research done on one’s own. Any questions are also welcome. Hopefully this also proves useful to others with MCAS.
Cheers for the best!