Anorexia is the decreased sensation of
appetite. While the term in non-scientific publications is often used interchangeably with
anorexia nervosa, many possible causes exist for a decreased appetite, some of which may be harmless, while others indicate a serious clinical condition or pose a significant risk.
For example,
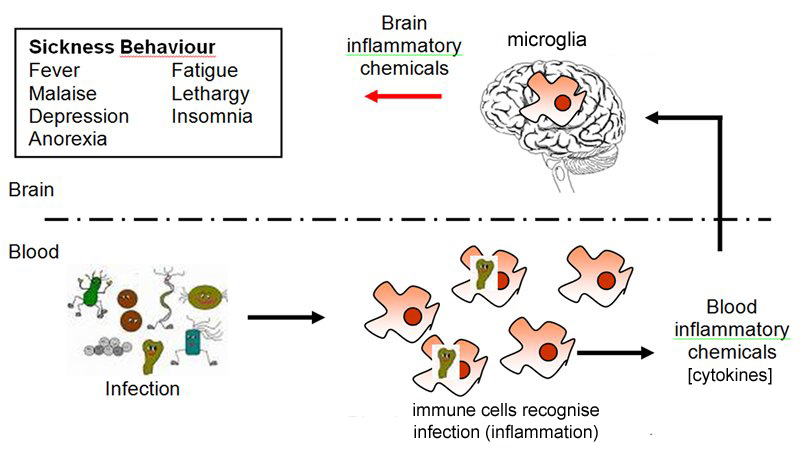
anorexia of infection is part of the
acute phase response (APR) to infection. The APR can be triggered by
lipopolysaccharides and
peptidoglycans from bacterial cell walls, bacterial DNA, double-stranded viral RNA, and viral
glycoproteins, which can trigger production of a variety of
proinflammatory cytokines. These can have an indirect effect on appetite by a number of means, including
peripheral afferents from their sites of production in the body, by enhancing production of
leptin from fat stores. Inflammatory cytokines can also signal to the
central nervous system more directly by specialized transport mechanisms through the
blood–brain barrier, via
circumventricular organs (which are outside the barrier), or by triggering production of
eicosanoids in the
endothelial cells of the brain vasculature. Ultimately the control of appetite by this mechanism is thought to be mediated by the same factors normally controlling
appetite, such as neurotransmitters (
serotonin,
dopamine,
histamine,
norepinephrine,
corticotropin releasing factor,
neuropeptide Y, and
α-melanocyte-stimulating hormone).
[1]