pattismith
Senior Member
- Messages
- 3,946
This study got my interest because:
1- muscle weakness is also a frequent feature in CFS/ME
2-COPD/Chronic Obstructive Pulmonary Disease) genes seem to be potential risk factor for Fibromyalgia (see here)
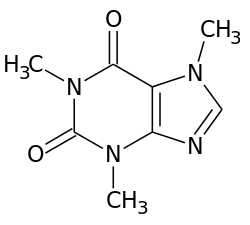
3-Inbalance between ATP/ADP/Adenosine was found in ME/CFS
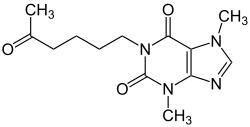
4-I solved my own muscle weakness when I took Inosine, a metabolite of IMP
https://www.atsjournals.org/doi/pdf/10.1164/ajrccm.157.2.9608064
1- muscle weakness is also a frequent feature in CFS/ME
2-COPD/Chronic Obstructive Pulmonary Disease) genes seem to be potential risk factor for Fibromyalgia (see here)
3-Inbalance between ATP/ADP/Adenosine was found in ME/CFS
4-I solved my own muscle weakness when I took Inosine, a metabolite of IMP
Elevated IMP Levels in Resting Muscle of Patients with Stable COPD said:Summary:
In summary, in patients with stable COPD elevated muscular IMP content was found under resting conditions. IMP levels were negatively related to the ATP/ADP ratio, suggesting an imbalance between ATP utilization and resynthesis. The fact that these abnormalities were already found under resting conditions suggests that muscular energy status in COPD patients might even be more compromised during exercise. The cause and consequences of these disturbances in muscle energy metabolism in COPD patients need further exploration
Intro:
Impaired exercise performance is a frequently occurring problem in patients with chronic obstructive pulmonary disease (COPD= chronic obstructive pulmonary disease) (1).
The two dominant symptoms limiting exercise tolerance in COPD are dyspnea and a sensation of fatigue in leg muscles (1).
Recently, it has been shown that both skeletal and respiratory muscle weakness contribute to the severity of these symptoms (2) and to reduced exercise tolerance, independent of lung function impairment (2, 3).
The cause of muscle weakness in COPD patients is incompletely understood. It has been shown that the development of muscle weakness is frequently associated with loss of body mass and in particular loss of muscle mass…
DIscussion:
In the present study, elevated muscular IMP levels and decreased ATP/ADP and PC/C ratios were found in patients with stable COPD compared with healthy control subjects under resting conditions. ATP, ADP, AMP, and TAN did not differ between patients and control subjects.
Within the patient group, two subgroups could be distinguished: a subgroup with muscular IMP content > 0.06 mmol/kg dry weight (IMP1 patients) and a subgroup with an IMP content , 0.06 mmol/kg dry weight (i.e., below the detection level) (IMP2 patients).
This division seemed relevant since only one of eight control subjects also had a measurable IMP content. In the IMP1 patients, lower ATP/ADP and PC/C ratios were found compared with IMP2 patients.
Clinically, IMP1 patients differed from IMP2 patients in that they had a significantly lower DLCO. IMP and ammonia (NH3) are produced during deamination of AMP (AMP→IMP 1 NH3).
...
In healthy subjects, IMP content in resting muscle is very low. Elevated IMP levels are only found during high intensity exercise (75% O2max) (8). Several studies in healthy subjects indicated that special conditions, such as hypoxemia (18) or V ·
initial shortage of muscular glycogen, induce enhanced IMP accumulation during exercise (19). It is generally believed that, in these acute situations, IMP formation reflects an imbalance between ATP utilization and resynthesis.
In the present study, we hypothesized, based on the previously observed changes in aerobic and glycolytic capacity (6, 7), that in patients with stable COPD alterations might occur in muscular high-energy phosphate concentrations.
Furthermore, we assumed that IMP measurements would enable us to detect subtle changes in muscular energy balance. Indeed, in this study, elevated IMP levels were found that were associated with lower ATP/ADP ratios. The finding of elevated IMP content in resting muscle, is to our knowledge, unique…
Because of the observed relationship between IMP content and ATP/ADP ratio, other explanations for the enhanced IMP content, such as disturbances in pathways catabolizing IMP (such as degradation of IMP to inosine and further) or disturbances in the purine nucleotide cycle (where IMP is reaminated to AMP), seem less relevant.
An imbalance between ATP utilization and resynthesis can be caused by enhanced ATP utilization, decreased ATP resynthesis, or both. Earlier studies by our group and others have shown that a significant proportion of COPD patients have increased resting energy expenditure (22).
Biopsies were obtained from the tibialis muscle using a conchotome. However, in all the studies quoted here, biopsies were taken from the quadriceps femoris muscle, which has a different fiber type distribution compared with the anterior tibialis muscle (40% and 70% type I fibers, respectively) (25). In healthy subjects during exercise, higher IMP formation has been found in type II fibers compared with type I fibers (8). Therefore, if quadriceps femoris muscle would have been used in this study, results might have been different
https://www.atsjournals.org/doi/pdf/10.1164/ajrccm.157.2.9608064
Last edited: