SDSue
Southeast
- Messages
- 1,066
I may have found what's been instrumental in helping my POTS. (Sorry - lengthy post)
Due to elevated liver enzymes, my doc asked me to wean off Mirtazapine (used as needed for sleep) as well as Famvir. (I've been completely off famvir for about a month, off mirtazapine for about 2 weeks)
I've been getting progressively worse during this time, to the point I'm back in bed. My POTS has been horrid. I blamed the lack of Famvir and viral reactivation, but I may have been wrong.
Last night, unable to sleep at all, I broke down and took half of a mirtazapine at 4:30 am. Today, my POTS is much better. Few palpitation, resting HR back under 60, even took a shower (sitting, of course, but it counts!) My question is this:
Does anyone know which of the following mechanisms of mirtazapine might be responsible for the control of POTS? I need to find a drug that can work without raising liver enzymes. (I failed on florinef, midodrine, salt and fluid loading) Needless to say, doctors are clueless and I need to guide mine in this process. What I wouldn't give for a good POTS doctor!!!
The following Mirtazapine mechanisms of action are from Drugs.com
5-HT3 antagonists include drugs used to combat chemo-incuded emesis.
Where's a good pharmacologist when we need one? Fortunately, it takes nearly 10 days for mirtazapine to completely clear the body, so it may be possible to take a low dose infrequently and still achieve clinically significant help with POTS. Side note: I have also on a very low dose of Atenolol for a few months, and that dose did not change during the above unintended "experiment".
Due to elevated liver enzymes, my doc asked me to wean off Mirtazapine (used as needed for sleep) as well as Famvir. (I've been completely off famvir for about a month, off mirtazapine for about 2 weeks)
I've been getting progressively worse during this time, to the point I'm back in bed. My POTS has been horrid. I blamed the lack of Famvir and viral reactivation, but I may have been wrong.
Last night, unable to sleep at all, I broke down and took half of a mirtazapine at 4:30 am. Today, my POTS is much better. Few palpitation, resting HR back under 60, even took a shower (sitting, of course, but it counts!) My question is this:
Does anyone know which of the following mechanisms of mirtazapine might be responsible for the control of POTS? I need to find a drug that can work without raising liver enzymes. (I failed on florinef, midodrine, salt and fluid loading) Needless to say, doctors are clueless and I need to guide mine in this process. What I wouldn't give for a good POTS doctor!!!
The following Mirtazapine mechanisms of action are from Drugs.com
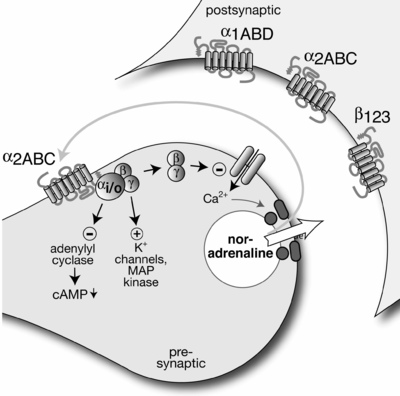
Yohimbine is in this class, but I think it's peripheral in action? It makes symptoms much worse!Evidence gathered in preclinical studies suggests that mirtazapine enhances central noradrenergic and serotonergic activity. These studies have shown that mirtazapine acts as an antagonist at central presynaptic α2–adrenergic inhibitory autoreceptors and heteroreceptors, an action that is postulated to result in an increase in central noradrenergic and serotonergic activity.
5-HT2 antagonists include ketanserin, an antihypertensive.Mirtazapine is a potent antagonist of 5-HT2 and 5-HT3 receptors. Mirtazapine has no significant affinity for the 5-HT1A and 5-HT1B receptors.
5-HT3 antagonists include drugs used to combat chemo-incuded emesis.
Drugs in this class include ketotifen, meclizine, and promethazine among others.Mirtazapine is a potent antagonist of histamine (H1) receptors, a property that may explain its prominent sedative effects.
Drugs include the antihypertensive Reserpine, thought to deplete sympathetic amines in both the central nervous system and periphery.Mirtazapine is a moderate α1–adrenergic antagonist, a property that may explain the occasional orthostatic hypotension reported in association with its use.
Includes mebeverine (IBS) trihexyphehidyl (anti-parkinson"s) diphenhydramine (good old Benadryl)Mirtazapine is a moderate antagonist at muscarinic receptors, a property that may explain the relatively low incidence of anticholinergic side effects associated with its use.
Where's a good pharmacologist when we need one? Fortunately, it takes nearly 10 days for mirtazapine to completely clear the body, so it may be possible to take a low dose infrequently and still achieve clinically significant help with POTS. Side note: I have also on a very low dose of Atenolol for a few months, and that dose did not change during the above unintended "experiment".