Dude
Senior Member
- Messages
- 190
Abstract
After a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, approximately 10-20% of patients are affected by the post-COVID syndrome (PCS). This condition leads to a variety of functional complaints, including symptoms of fatigue. To date, there is still no adequate treatment option. Five patients are presented, including the self-observation of one of the authors, in whom the administration of amifampridine as an "off-label use" led to a normalization of the unphysiologically increased need for sleep with a simultaneous increase in the Bell score. This effect was confirmed in a double-blind discontinuation trial (the medication was discontinued on a trial basis) in two of the patients. The five patients, who were previously unable to lead a normal life due to their fatigue symptoms, were able to return to everyday life after treatment with amifampridine. This offers hope to millions of affected patients.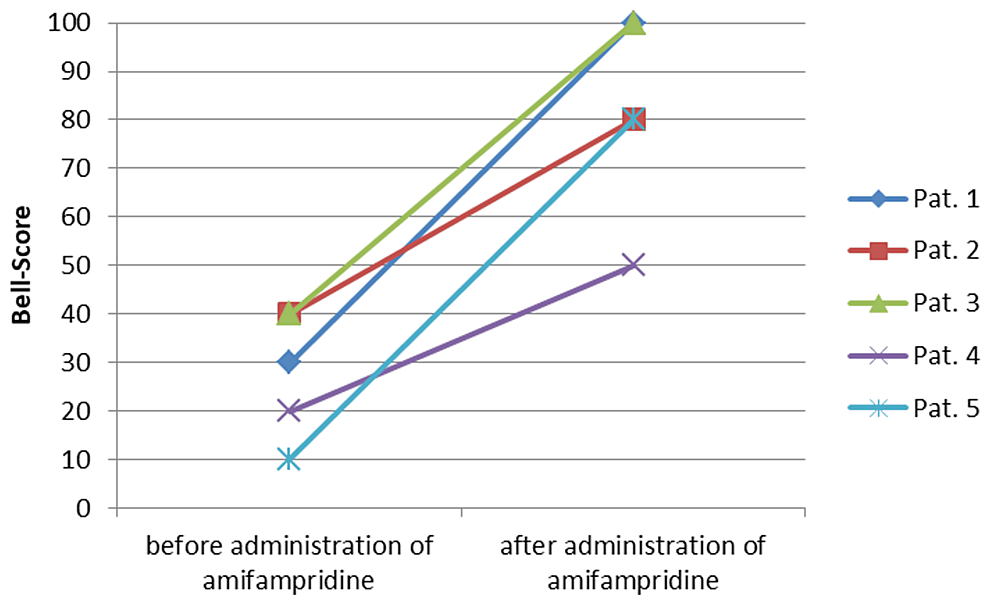
https://www.cureus.com/articles/218...y-with-double-blind-discontinuation-trials#!/
