View the Post on the Blog
View the Post on the Blog
Simon McGrath examines the latest research publication from Professor Baraniuk and Dr Rayhan
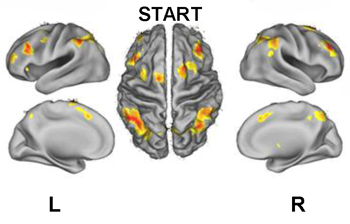
An fMRI image showing activation of brain areas during a cognitive test. From the PLoS One paper
Exercise challenge is fast the becoming THE key method when studying illnesses characterised by Post Exertional Malaise, such as Gulf War Illness (GWI) and ME/CFS. A paper just published looks at how exercise affects pain, cognitive performance, heart rate and brain functioning in patients with GWI. These patients also happened to meet the criteria for CFS, albeit only based on questionnaire diagnosis, making this study particularly interesting from an ME/CFS perspective.
Professor James Baraniuk and his colleague Dr Rakib Rayhan actually used a repeat challenge, with bicycle exercise on successive days, and looked for differences between 28 GWI patients and 10 controls, both before exercise and after. What they found was...initially, not much, it seems.
Pain was higher at baseline in GWI patients, as expected given that pain is one of the symptoms of GWI. And it appears that pain for GWI patients got worse after exercise, unlike controls. But they didn't find the expected drop off in performance on the exercise bike at the second test (this fits with the latest results for CFS patients presented by Christopher Snell at the FDA workshop). And cognitive performance didn't deteriorate after exercise (it was already low) - and brain functioning wasn't so different either. Overall, increase in heart rate on standing (POTS) was unaffected by exercise too.
Detective work pays off

Dr Rakib Rayhan
The study looked like a disappointment, until Rakib Rayhan did some digging through the data and noticed a marked difference amongst GWI patients. One subgroup (of 10 patients) showed tachycardia on standing (POTS) after exercise, while the remainder, 18, did not. The tachycardia patients, dubbed START for "Stress Test Associated Reversible Tachycardia", also had much higher levels of anxiety and other problems such as gastrointestinal symptoms. The other GWI subgroup, labelled STOPP (with the PP standing for 'Phantom Perception' of pain), had an increase in pain after exercise compared with controls. However, the STOPP group pain increase doesn't appear to be significantly different from START, and I suspect the label was chosen mainly because it makes a snappy acronym(though see below for some fMRI evidence that extra 'pain' regions are activated in STOPP patients).
What made these START and STOPP groups so interesting was that when they re-analysed the fMRI data they found the two groups had very different brain activation patterns during cognitive testing, and the patterns changed in a different way for each subgroup after exercise. For controls, the expected brain areas assoicated with working memory lit up during pre-exercise memory testing, but GWI patients activated these areas and aditional ones too (a similar phenomenon has been seen in CFS patients); it's possible that GWI patients needed to use more brain areas to get the same job done. Intriguingly, START and STOPP groups activated different additional areas. After exercise, there was less activation in the brain of controls as well as GWI patients, and bizarrely no activation in the START group.
Try a version of the working memory test used in this study
Intriguingly, for the STOPP group, the additional regions lighting up in response to cognitive exercise increased are play important roles in processing pain perception. Before exercise the extra activity was in the bilateral anterior insula, after exercise it was the medial frontal gyrus. However, these regions have functions other than pain perception too so their activation may not relate to pain perception.
Rayhan and Baraniuk also looked at brain structure, and found lower volumes of grey and white matter in certain regions compared with controls - again the pattern was different for START and STOPP patients.
The researchers theorise that these differences in post-exercise tachycardia, brain functioning and brain structure mark out two distinct phenotypes. Which is amazing as originally they'd thought the tachycardia testing wouldn't go anywhere: "I thought this would be a waste of the nursing staff's time," said James Baraniuk, adding that they did not expect the veterans to be different from the control group – or for there to be subgroups within the veterans. Instead, "It became a fundamental way of splitting the two veteran groups".
Except...
Other experts are less convinced, noting that most of the subjects in the Georgetown study were self-selected and that their number was relatively small: 28 veterans with symptoms and 10 participants without symptoms. For the START subgroup, the comparison was between 10 controls and 10 patients and findings on such small samples can prove unreliable. Also, the authors say the bizarre finding of no brain activation during cognitive testing post-exercise may be an artefact of their method - but presumably some of the other findings could be artefacts too. The results need verifying.
Dr Drew A Helmer, director of the Department of Veterans Affairs’ War-Related Illness and Injury Study Center, called the Georgetown studies “very preliminary” but also “a very important step forward.”
Replication (as always) is key
The authors themselves emphasise the need for replication and validation, and they are hoping to get funding for a replication study on a new sample of patients. Given Dr Helmer's comments on the potential importance of the findings, perhaps his Department will fund the work. The results from this will give a far clearer picture of whether or not there are indeed two types of GWI patients - if there are, it could prove very important indeed, as they note:
Identifying biomarkers such as these for phenotypic designation is one way to begin untangling the pathophysiological and molecular mechanisms underlying idiopathic disease states such as Gulf War Illness.
Those idiopathic illnesses, of course, include ME/CFS.
Update on the replication study, and relevance to CFS, from Dr Rakib Rayhan on Monday 1 July:
We are hopeful that this leads to a replication study in the near future. Ideally, we would like a very large sample of controls and GWI subjects for greater power and validation of current findings. Due to the overlap in symptomology, we feel that this protocol of brain scans before and after exercise perturbation holds tremendous promise to possibly try to understand central nervous system mechanisms in CFS.
Simon McGrath tweets about ME/CFS Research Follow @sjmnotes
Phoenix Rising is a registered 501 c.(3) non profit. We support ME/CFS and NEID patients through rigorous reporting, reliable information, effective advocacy and the provision of online services which empower patients and help them to cope with their isolation.
There are many ways you can help Phoenix Rising to continue its work. If you feel able to offer your time and talent, we could really use some more authors, proof-readers, fundraisers, technicians etc. and we'd love to expand our Board of Directors. So, if you think you can help then please contact Mark through the Forum.
And don't forget: you can always support our efforts at no cost to yourself as you shop online! To find out more, visit Phoenix Rising’s Donate page by clicking the button below.
View the Post on the Blog

