- Messages
- 86
- Location
- East of England
Back streaming
My mother is an expert in family therapy - has run family therapy department in the NHS for years - and I'm certain she would say this idea is a nonsense when it comes to true cases of ME/CFS.I laughed out loud at the "family-based approaches to treatment" bit because it's clearly hinting at family therapy. Interesting data nonetheless. Looks like there may be a role for the mother's diseased microbiome being passed on to the child at that crucial early age, setting them up for problems later on when puberty hits.
Probably a reference to this:Which autoantibodies?
The Simon Collin talk 'Cohort Profile: The Collaborative on Fatigue Following Infection (COFFI)' was intriguing. It aims to set up an international consortium of post-infectious cohorts, looking at post-infectious fatigue (including but not restricted to mecfs)
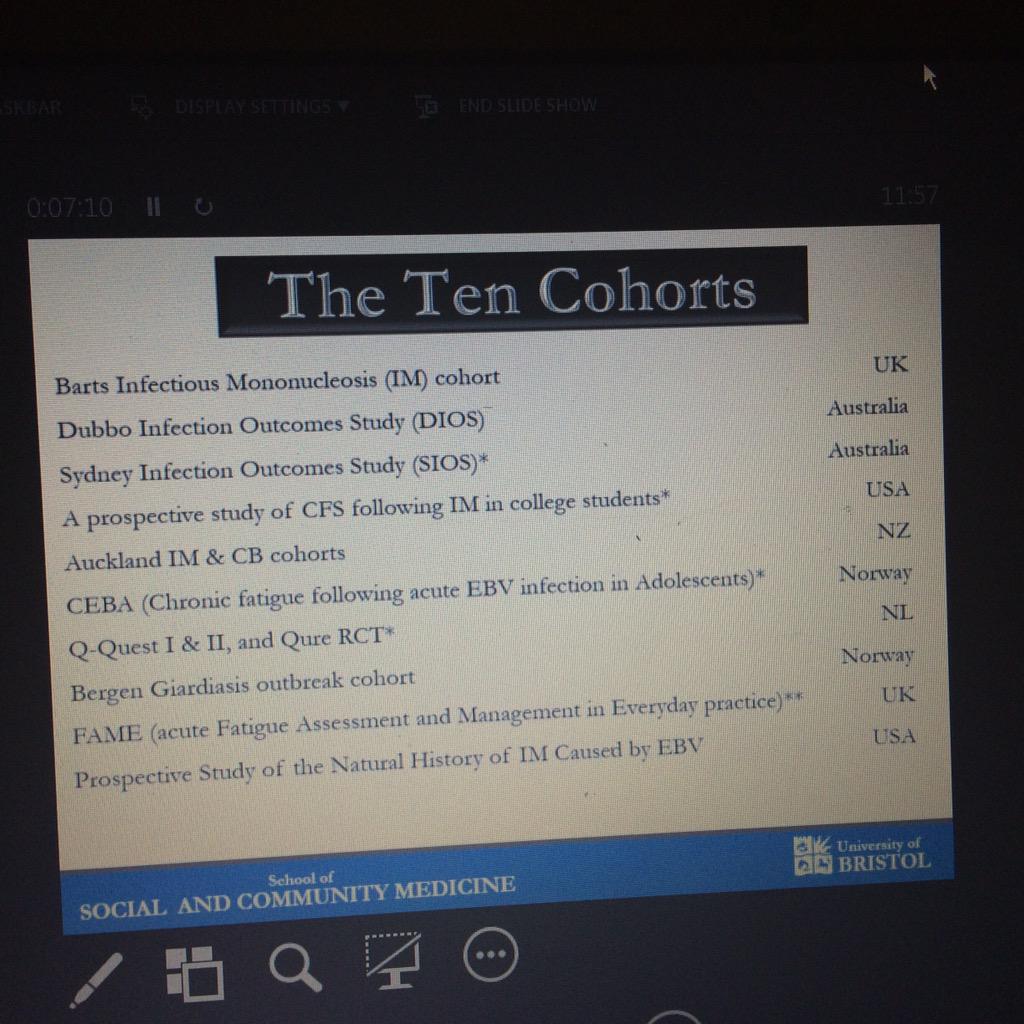
So, I know a lot of people will be suspicous of a project driven by Esther Crawley, Peter White and Andrew Lloyd. But there are some really interesting things about this study, not least that it's huge, and includes the Dubbos cohort (one of my favourite studies), the Katz/Jason huge NIH-funded prospective study of glandular fever in college students and the intriguing Bergen Giardia outbreak (Giardia lambia is a nasty gut parasite) that led to many cases of IBS and CFS.
Also, Collin said there had been an attempt several years ago to construct a huge UK cohort, including a Gene Wide Association Study, that failed to get funding. You could see that as one arm of the Grand Challenge mapped out by Stephen Holgate, that would add gene expression, proteomics, metabalomics and immune profiling (and more) to this approach. The feedback from rejected grant applications was that the combination of a) a broad and disputed case definition - and almost certainly a lot of patient heterogeneity (ie probably lots of different illnesses), coupled with b) the lack of specific hypotheses made it too vague. They hoped by focusing on post-infectious cases (getting in at the beginning of the illness too) they would have a much 'cleaner' patient cohort, combined with much greater statistical power (ie ability to find real effects) from a huge group of cohorts, would given them more chance. Potentially patients (the mecfs ones) from this international consortium could be just what's needed for the Grand Challenge and other studies.
Probably a reference to this:
Antibodies to ß adrenergic and muscarinic cholinergic receptors in patients with CFS
http://forums.phoenixrising.me/index.php?threads/antibodies-to-ß-adrenergic-and-muscarinic-cholinergic-receptors-in-patients-with-cfs.40109/
In relation to CFS, I think most BPS researchers may be abandoning the symptom-focusing hypothesis because it isn't supported by research. e.g. It hasn't been supported by the follow-up PACE analyses.symptom-focusing
Except that Prof Newton appears to study dysautonomia, not ME (and can't distinguish the two, apparently). So what she discovers for dysautonomia patients in general may not apply reliably to PWME.On Julie Newton's talk (latest tweet first):
Good to be back to biomedical stuff...
Yes, Newton does have a specialist interest in fatigue, but are you sure it's accurate to say that she doesn't study ME/CFS at all? Her studies do include CFS patients.Prof Newton needs to stop claiming she is researching (and treating) ME/CFS and be clear that she's actually studying generalized fatigue and dysautonomia. Her research in those areas is valuable and deserves the credit it gets.
I don't think it's widely recognised in the UK. Almost the only time I've ever seen it mentioned is on these forums, and I had to look up its meaning.Dysautonomia is an important field that needs more research and clinicians. I'm not sure why she's glommed onto ME/CFS when dysautonomia is less controversial. Or is dysautonomia not a recognized condition in the UK?
I don't think it's widely recognised in the UK. Almost the only time I've ever seen it mentioned is on these forums, and I had to look up its meaning.
This would only be useful if they were actually looking at the post-infective physiology. Given that Crawley, White, and Lloyd are involved, I think we can safely assume that the research will take as a given that the reason for the fatigue is psychological. If you start with an unproven (and in this case incorrect) assumption, it's pretty much guaranteed that the biases in your study design combined with the way you interpret the results based on your false assumption will lead to invalid conclusions.The Simon Collin talk 'Cohort Profile: The Collaborative on Fatigue Following Infection (COFFI)' was intriguing. It aims to set up an international consortium of post-infectious cohorts, looking at post-infectious fatigue (including but not restricted to mecfs)
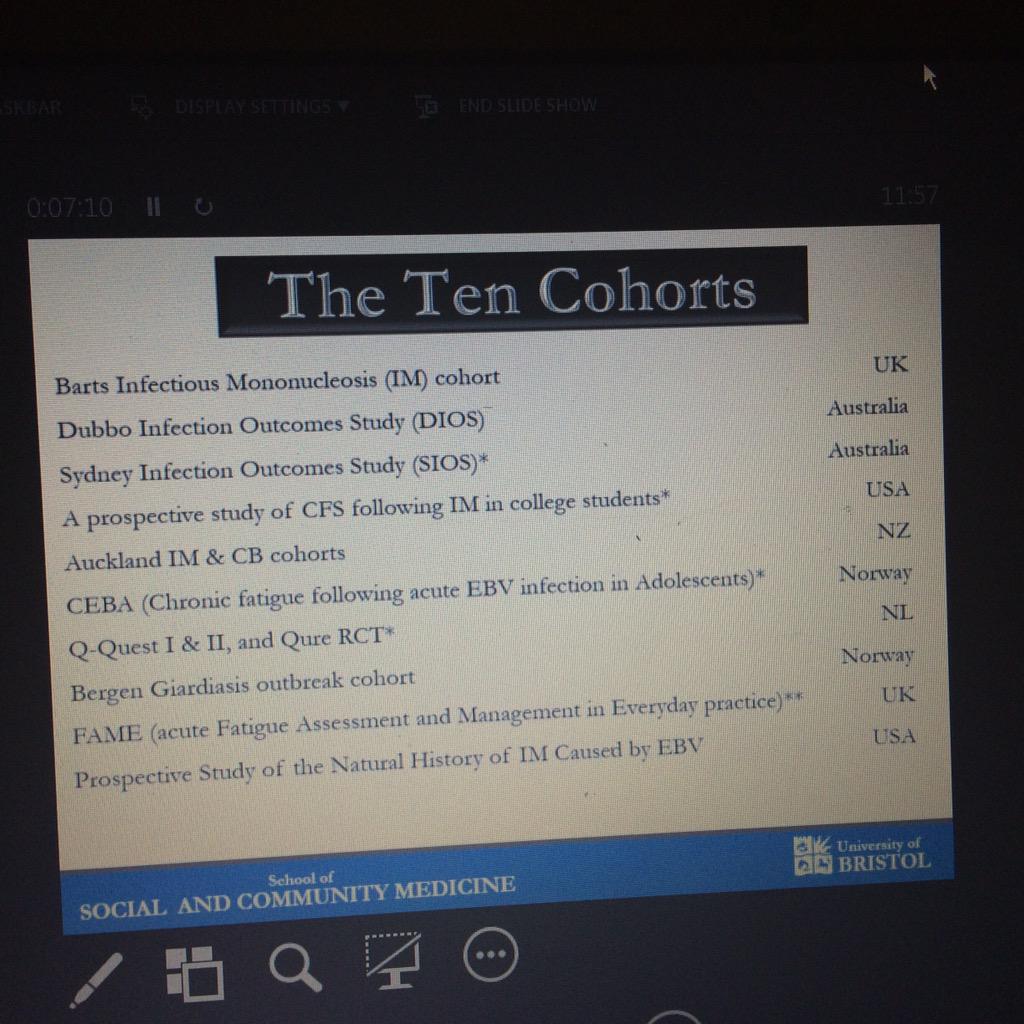
So, I know a lot of people will be suspicous of a project driven by Esther Crawley, Peter White and Andrew Lloyd. But there are some really interesting things about this study, not least that it's huge, and includes the Dubbos cohort (one of my favourite studies), the Katz/Jason huge NIH-funded prospective study of glandular fever in college students and the intriguing Bergen Giardia outbreak (Giardia lambia is a nasty gut parasite) that led to many cases of IBS and CFS.
Don't think about pink Elephants...'fraid I had to.To all members of this forum... DON'T DON'T DON'T look at this document.. Just don't. I can't quite believe what I've just seen.
How does she define a CFS patient? Reading her research suggests she conflates chronic fatigue with OI and ME/CFS.Yes, Newton does have a specialist interest in fatigue, but are you sure it's accurate to say that she doesn't study ME/CFS at all? Her studies do include CFS patients.
Here, have some brain soap.Don't think about pink Elephants...'fraid I had to.
How does she define a CFS patient? Reading her research suggests she conflates chronic fatigue with OI and ME/CFS.
Sadly, anybody can say they are studying CFS without any real verification that the patient has anything more than self-reported chronic fatigue of the mildest sort.