Stool tests can't identify SIBO and if yours didn't come with a yeast culture, you could be missing candida as well.
I think stool testing provides a lot of great information, for me personally, they helped me identify a Candida kruseii overgrowth and some protozoa whose significance is debated, but clearing up both improved my brain fog. The fatty acid, inflammation markers, and digestive chemistries are also helpful
That said, I think there are some inherent challenges with stool tests. While there are a few bacteria that stand out as key pathogens an opportunist, for the most part, gut health isn't about a specific bacteria, but about how they behave as a community. I had an eye opening experience when a colleague and I both did GI-MAP tests (these provide a long list of microbes identified via PCR) one month apart and found that there was very little consistency in which bacteria where marked as high and low.
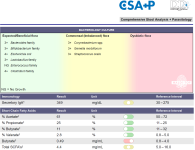
Scientists are beginning to look at the microbiome in terms of patterns instead of just single bacteria. Doctor's Data (no I am not affiliated with them) has a test called GI360 which looks at an abundance and diversity pattern across multiple bacterial phyla, classes, family, genus, and species levels to distinguish a dysbiotic microbiome from a normobiotic. What is nice about it is that the dysbiotic patterns have been verified in multiple clinical trials and verified for reproducibility, so even if some bacteria go up or down on repeat testing, the dysbiotic pattern remains. However, even though this test is probably the best out there for identification of dysbiosis, it still doesn't identify exactly which bacteria are the problem. You can see the levels of all the bacteria tested, but it is the pattern that is the issue.