- Messages
- 22
@Murph, give me a moment and I'll try to see what I can do! (Ideally today!) Lol! Because yes I can see how this is really long and/or difficult to read. 
But yes, I do think that PEM might be an activation of the immune system, more precisely a pseudo-allergic reaction to physical exercise. I'll try to summarize the key points so it's a few lines / paragraphs and not 5 pages.
@anciendaze, I didn't mean to say that rhabdomyolysis is not mast cell mediated, or incompatible with the PEM experienced by patients that receive a CFS/ME diagnosis.
It's just that even at the very worse of my illness, and even during the CPET where I pushed my body to the very limits of where I could go:
- I don't remember my CK levels having ever been elevated (though I'll admit no blood was drawn during the exercise itself, I'd have to ask Dr. Betsy Keller if abnormally elevated CK levels have ever been noted in her group of patients during and/or following exertion),
- I don't experience pain, just a very light soreness in my legs. And I don't feel actually out of breath that much. What stops me from continuing to do the exercise when I reach my VO2 Max is that my muscles are so tired they are refusing to contract! I told Dr. Keller "I could have continued if my legs had just agreed to keep pushing those pedals!" and she laughed and answered "Oh no girl, you're toast! You've given all you could give without actually killing yourself!"
- I've never had any kidney issues (that I know of).
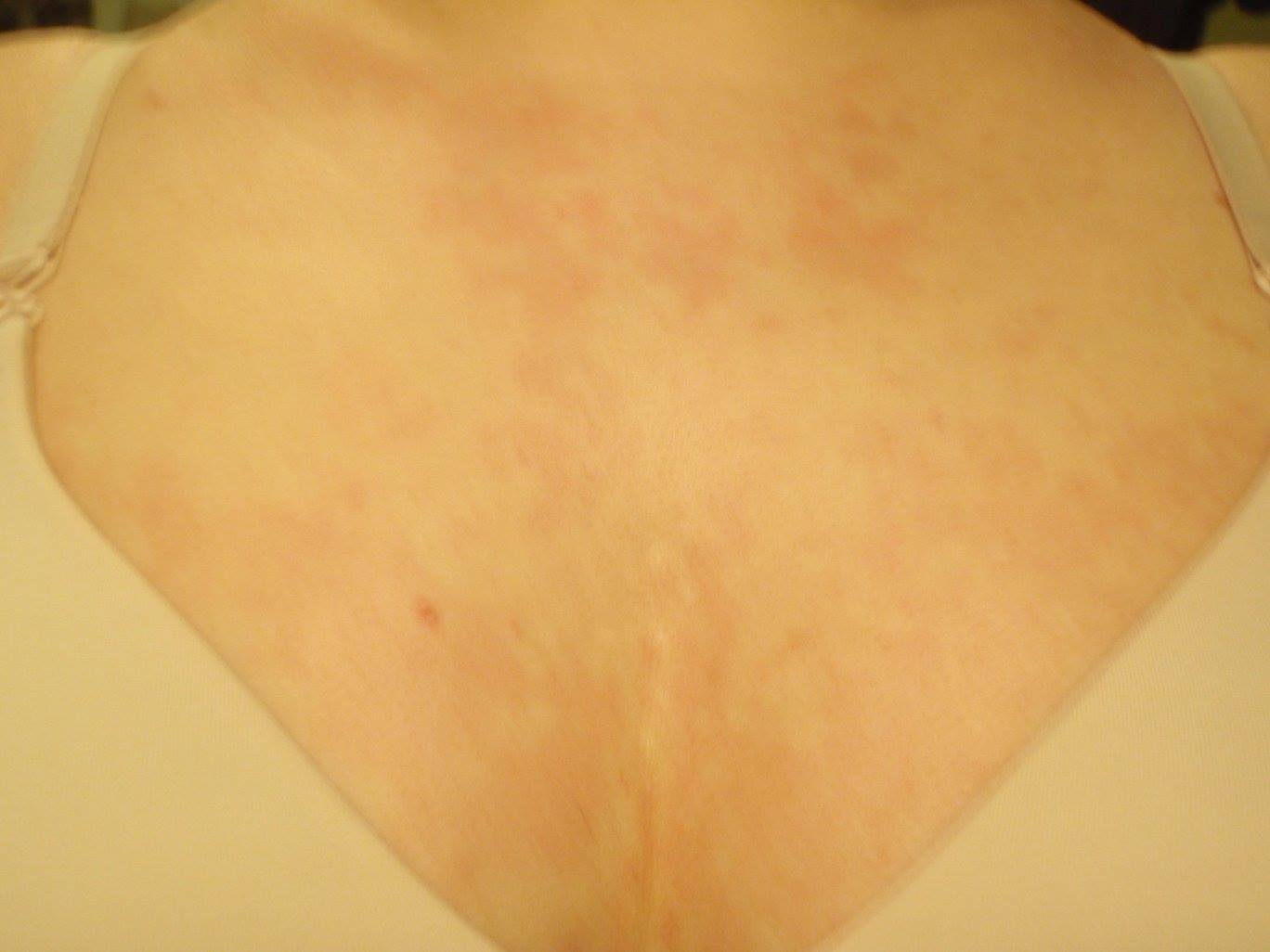
- Exercise triggers malaise and a pseudo-allergic reaction, but the symptoms are largely the same ones I experience as when I eat certain foods, or go out in the sunshine, or am exposed to the vibrations of a car, or then again certain smells.
And through mast cell degranulation in response to those triggers there is some mitochondrial ATP and DNA released in the blood by the mast cell themselves.
Then again, from what I'm reading right now, rhabdomyolysis seems to be happening in response to other triggers besides physical exertion. Like food, heat or cold, etc.
So I can't deny there are huge similarities.
I guess it's just that I do have muscle weakness (hence why we suggested that I might be suffering from DOK7 congenital myasthenia), but my CK levels have been consistently fine, EMG came back perfectly normal...
Like we've never clinically observed any sign of muscle destruction or injury. Actually, one of the things that cued the neurogeneticist I might have DOK7 congenital myasthenia was the fact that I had surprisingly developed and strong muscles for someone who'd been homebound for about 5 years at the time.
I muscle mass loss and tone was extremely minimal. However, if you asked me to quickly contract my muscle (by bending the elbow in 2, and flapping my arm like a chicken wing) 10 times, and then try lift and keep my arm parralel to the ground while he lightly pushed down on it, it's like that muscle had completely vanished and I could offer no resistance.
At rest, it was no issue at tall, he could almost put all his weight on the arm and it would not bulge. Flap it 10 times? Muscle tone? Gone!
But it was just gone and the arm didn't hurt nor did I sense any other discomfort.
Actually, my muscles tend to be sore and tense in the morning when I wake up, but then during the day the more I move, the more the pain goes down. Though I do experience joint pain up to a certain level (but not enough to affect my range of motion or stop me from being able to move).
What we've found by putting an infrared camera in the bedroom, is that I can do from 30 to about 150 stereotyped movements per night where I will raise my legs, cross and uncross them in the air, raise my arm like a Hitler salute (a classical sign of frontal lobe seizure according to Dr. Hyde) and keep it there for a few minutes, interact with my pillow and environment, put my hands in the pockets of my PJ (if they have pockets), remove them from the pockets, put my hands in my pockets, remove them from my pockets, and so forth.
Sometimes, you can clearly see the muscles just contract hard and go through spasms for no apparent reason. And I'll clench my jaw so hard (while also modifying its position) that I've managed to break some of my enamel (I now wear a nightguard).
So basically, we've concluded that the muscle pain and discomfort I experience (and that has been diagnosed as fibromyalgia) might just be caused by all those movements I make every night.
But, while there is some odd electrical activity happening day and night in my left temporal lobe, it seems that as soon as you put me in a clinical setting like this, I stop moving. I do experience multiple micro-awakenings without any observable reasons, though.
So perhaps I have a poor understanding of what rhabdomyolysis is, but I'm not sure I'd fit the diagnostic criteria...
The joint pain and muscles soreness did not go down since receiving the Xolair (Omalizumab) injections, it sort of went up a bit, actually, because I'm regularly exercising, belly dancing 1 hour every day, and so forth. So my muscles are a lot more solicited than they used to be, and I've developed more tensions in new places (my massotherapist is having a blast with my abdominal wall!).
Just like, oddly enough, I do have some "traits" of EDS type III, but not enough to fit the criteria, either.
Like I can touch my forearm with my thumb, I have easy bruising, a high and narrow palate, functional bowel disorder, easy bruising, chronic joint pain...
As a child I likely would have met the criteria given the hypermobility (that is still present in some articulations, like the knees that bend more than 180 degrees), and the fact that I really tended to easily dislocate and/or experience subluxation in certain articulations. As a teenager I had to wear knee braces otherwise I would sometimes collapse when I ran.
But I can't even touch the floor anymore with my knees straight. I'm able to bring a single foot behind my head, while I used to be able to bring both legs behind the small of my back.
So yes, I do have a history of hypermobility, but now it's very much restricted so certain angles and/or articulations. And not enough to warrant an EDS diagnosis according to the doctors.
Even my dysautonomia isn't a passive or positional process. So the tilt-table test was perfectly fine. But it's when I had to make the physical effort to go from a lying down to sitting, or sitting to standing position that the values on my heart rate monitor would suddenly rise more than 40 bpm.
So, like you've said, since there are a lot of mast cells lining the blood vessels and in the connective tissues, I've always assumed that was more or less because the mast cells were triggering vasodilatation and increased blood vessel permeability in response to physical effort, and my heart was beating faster to compensate for the blood pressure drop.
Which is sort of what my CPET showed - i.e. that my blood pressure fails to increase with physical activity.
I think that explains why I really tended to associate PEM with a transient allergic reaction... Though then again, rhabdomyolysis might be taking that reaction one step further...
http://criticalcareshock.org/files/Anaphylaxis-and-rhabdomyolysis.-Any-early-relationship.pdf
Like you've said, the body is a very dynamic environment, and is not as "clear cut" as some specialists then to believe it is. All the systems are interacting together so you can't quite look at what the heart is doing without also looking a the brain and immune system.
The model I've presented earlier to tie EIA and PEM together is a very "naïve" and extremely oversimplified one. There are likely tons of other things happening while the mast cells are degranulating and tons of other organs and bodily structures being involved.
I'd never heard of rhabdomyolysis before, actually, so I'm still trying to figure out how and what's happening. I'm just wondering if skeletal muscles breaking down like that is something happening even in cases like me, that aren't consciously aware that there's something wrong happening with their muscles during exercise (besides feeling like they are simply refusing to contract anymore).
Or could it be what protects me from developing rhabdomyolysis in response to physical exertion? My muscles will just stop obeying orders and fail to contract before actual muscle injury has a chance to occurs?
Omalizumab binds itself to the IgE, thus preventing them from stimulating FceRI receptors on the surface of mast cells and triggering the allergic reaction.
It would also bind itself to the membrane IgE on B cells, decreasing B cells numbers and putting them in a state of anergy. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3875359/
But its exact mechanism of action as a mast cell stabilizer remains poorly known, given that it has been reported to be highly effective in cases of MCAS that did not present with elevated IgE levels.
However, it has been suggested that the FceRI receptors on mast cells and basophils become downregulated as well ( https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3340573/pdf/nihms-365715.pdf ), and that Omalizumab may interact with some mast cell mediators.
I've often wondered how I would have responded to Rituximab treatments given that it has been reported to induce remission in Idiopathic Anaphylaxis (IA) cases.
Though given that Omalizumab is probably safer and easier to be administered than Rituximab (subcutaenous injections v.s. intravenous administration) I'm rather glad I started with this one and responded so well to it!
Hope your move went well, and you won't have to suffer from a long recovery following this. I'm really glad you had help, too!
But yes, I do think that PEM might be an activation of the immune system, more precisely a pseudo-allergic reaction to physical exercise. I'll try to summarize the key points so it's a few lines / paragraphs and not 5 pages.
@anciendaze, I didn't mean to say that rhabdomyolysis is not mast cell mediated, or incompatible with the PEM experienced by patients that receive a CFS/ME diagnosis.
It's just that even at the very worse of my illness, and even during the CPET where I pushed my body to the very limits of where I could go:
- I don't remember my CK levels having ever been elevated (though I'll admit no blood was drawn during the exercise itself, I'd have to ask Dr. Betsy Keller if abnormally elevated CK levels have ever been noted in her group of patients during and/or following exertion),
- I don't experience pain, just a very light soreness in my legs. And I don't feel actually out of breath that much. What stops me from continuing to do the exercise when I reach my VO2 Max is that my muscles are so tired they are refusing to contract! I told Dr. Keller "I could have continued if my legs had just agreed to keep pushing those pedals!" and she laughed and answered "Oh no girl, you're toast! You've given all you could give without actually killing yourself!"
- I've never had any kidney issues (that I know of).
- Exercise triggers malaise and a pseudo-allergic reaction, but the symptoms are largely the same ones I experience as when I eat certain foods, or go out in the sunshine, or am exposed to the vibrations of a car, or then again certain smells.
And through mast cell degranulation in response to those triggers there is some mitochondrial ATP and DNA released in the blood by the mast cell themselves.
Then again, from what I'm reading right now, rhabdomyolysis seems to be happening in response to other triggers besides physical exertion. Like food, heat or cold, etc.
So I can't deny there are huge similarities.
I guess it's just that I do have muscle weakness (hence why we suggested that I might be suffering from DOK7 congenital myasthenia), but my CK levels have been consistently fine, EMG came back perfectly normal...
Like we've never clinically observed any sign of muscle destruction or injury. Actually, one of the things that cued the neurogeneticist I might have DOK7 congenital myasthenia was the fact that I had surprisingly developed and strong muscles for someone who'd been homebound for about 5 years at the time.
I muscle mass loss and tone was extremely minimal. However, if you asked me to quickly contract my muscle (by bending the elbow in 2, and flapping my arm like a chicken wing) 10 times, and then try lift and keep my arm parralel to the ground while he lightly pushed down on it, it's like that muscle had completely vanished and I could offer no resistance.
At rest, it was no issue at tall, he could almost put all his weight on the arm and it would not bulge. Flap it 10 times? Muscle tone? Gone!
But it was just gone and the arm didn't hurt nor did I sense any other discomfort.
Actually, my muscles tend to be sore and tense in the morning when I wake up, but then during the day the more I move, the more the pain goes down. Though I do experience joint pain up to a certain level (but not enough to affect my range of motion or stop me from being able to move).
What we've found by putting an infrared camera in the bedroom, is that I can do from 30 to about 150 stereotyped movements per night where I will raise my legs, cross and uncross them in the air, raise my arm like a Hitler salute (a classical sign of frontal lobe seizure according to Dr. Hyde) and keep it there for a few minutes, interact with my pillow and environment, put my hands in the pockets of my PJ (if they have pockets), remove them from the pockets, put my hands in my pockets, remove them from my pockets, and so forth.
Sometimes, you can clearly see the muscles just contract hard and go through spasms for no apparent reason. And I'll clench my jaw so hard (while also modifying its position) that I've managed to break some of my enamel (I now wear a nightguard).
So basically, we've concluded that the muscle pain and discomfort I experience (and that has been diagnosed as fibromyalgia) might just be caused by all those movements I make every night.
But, while there is some odd electrical activity happening day and night in my left temporal lobe, it seems that as soon as you put me in a clinical setting like this, I stop moving. I do experience multiple micro-awakenings without any observable reasons, though.
So perhaps I have a poor understanding of what rhabdomyolysis is, but I'm not sure I'd fit the diagnostic criteria...
The joint pain and muscles soreness did not go down since receiving the Xolair (Omalizumab) injections, it sort of went up a bit, actually, because I'm regularly exercising, belly dancing 1 hour every day, and so forth. So my muscles are a lot more solicited than they used to be, and I've developed more tensions in new places (my massotherapist is having a blast with my abdominal wall!).
Just like, oddly enough, I do have some "traits" of EDS type III, but not enough to fit the criteria, either.
Like I can touch my forearm with my thumb, I have easy bruising, a high and narrow palate, functional bowel disorder, easy bruising, chronic joint pain...
As a child I likely would have met the criteria given the hypermobility (that is still present in some articulations, like the knees that bend more than 180 degrees), and the fact that I really tended to easily dislocate and/or experience subluxation in certain articulations. As a teenager I had to wear knee braces otherwise I would sometimes collapse when I ran.
But I can't even touch the floor anymore with my knees straight. I'm able to bring a single foot behind my head, while I used to be able to bring both legs behind the small of my back.
So yes, I do have a history of hypermobility, but now it's very much restricted so certain angles and/or articulations. And not enough to warrant an EDS diagnosis according to the doctors.
Even my dysautonomia isn't a passive or positional process. So the tilt-table test was perfectly fine. But it's when I had to make the physical effort to go from a lying down to sitting, or sitting to standing position that the values on my heart rate monitor would suddenly rise more than 40 bpm.
So, like you've said, since there are a lot of mast cells lining the blood vessels and in the connective tissues, I've always assumed that was more or less because the mast cells were triggering vasodilatation and increased blood vessel permeability in response to physical effort, and my heart was beating faster to compensate for the blood pressure drop.
Which is sort of what my CPET showed - i.e. that my blood pressure fails to increase with physical activity.
I think that explains why I really tended to associate PEM with a transient allergic reaction... Though then again, rhabdomyolysis might be taking that reaction one step further...
http://criticalcareshock.org/files/Anaphylaxis-and-rhabdomyolysis.-Any-early-relationship.pdf
Like you've said, the body is a very dynamic environment, and is not as "clear cut" as some specialists then to believe it is. All the systems are interacting together so you can't quite look at what the heart is doing without also looking a the brain and immune system.
The model I've presented earlier to tie EIA and PEM together is a very "naïve" and extremely oversimplified one. There are likely tons of other things happening while the mast cells are degranulating and tons of other organs and bodily structures being involved.
I'd never heard of rhabdomyolysis before, actually, so I'm still trying to figure out how and what's happening. I'm just wondering if skeletal muscles breaking down like that is something happening even in cases like me, that aren't consciously aware that there's something wrong happening with their muscles during exercise (besides feeling like they are simply refusing to contract anymore).
Or could it be what protects me from developing rhabdomyolysis in response to physical exertion? My muscles will just stop obeying orders and fail to contract before actual muscle injury has a chance to occurs?
Omalizumab binds itself to the IgE, thus preventing them from stimulating FceRI receptors on the surface of mast cells and triggering the allergic reaction.
It would also bind itself to the membrane IgE on B cells, decreasing B cells numbers and putting them in a state of anergy. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3875359/
But its exact mechanism of action as a mast cell stabilizer remains poorly known, given that it has been reported to be highly effective in cases of MCAS that did not present with elevated IgE levels.
However, it has been suggested that the FceRI receptors on mast cells and basophils become downregulated as well ( https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3340573/pdf/nihms-365715.pdf ), and that Omalizumab may interact with some mast cell mediators.
I've often wondered how I would have responded to Rituximab treatments given that it has been reported to induce remission in Idiopathic Anaphylaxis (IA) cases.
Though given that Omalizumab is probably safer and easier to be administered than Rituximab (subcutaenous injections v.s. intravenous administration) I'm rather glad I started with this one and responded so well to it!
Hope your move went well, and you won't have to suffer from a long recovery following this. I'm really glad you had help, too!