pattismith
Senior Member
- Messages
- 3,946
AB0887 Jia patients with high disease activity have increased activity of both the ido and gtp-ch1 pathway, but decreased bh4 efficacy: consequences for fatigue and well-being
2019
Abstract
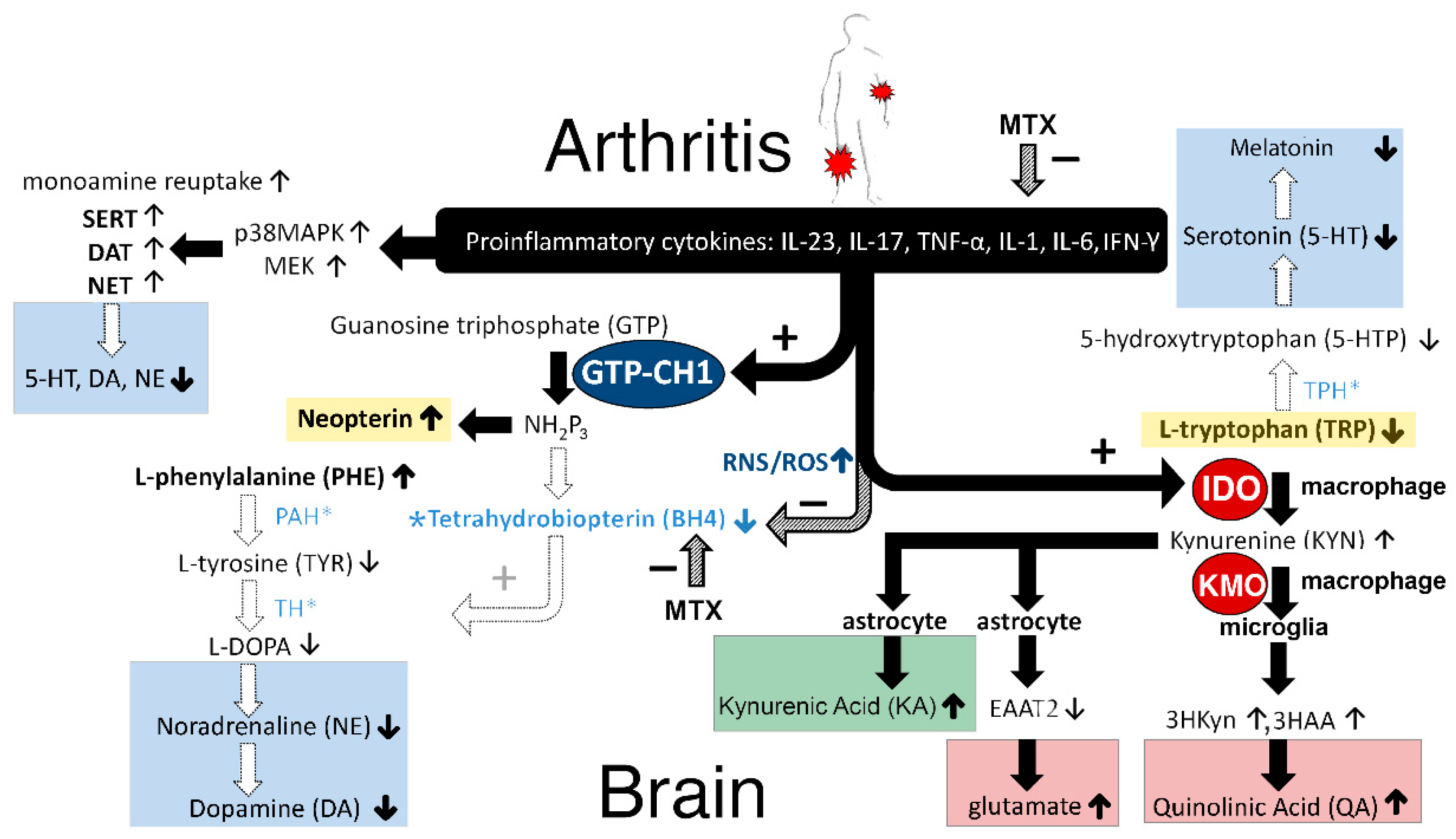
Background Juvenile idiopathic arthritis (JIA) patients suffer from an inflammatory condition, resulting in painful joints. In addition, JIA patients often report symptoms of sickness behaviour, including depressive symptoms and fatigue. Recent animal studies suggest that proinflammatory cytokines produce sickness behaviour by increasing the activity of indoleamine-2,3-dioxygenase (IDO) and guanosinetriphosphate-cyclohydrolase-1 (GTP-CH1). Here it is hypothesised that inflammation in JIA patients affects the enzymatic activity of IDO and GTP-CH1 and the co-factor BH4. These compounds play a crucial role in the metabolism of the neurotransmitters serotonin and dopamine.
Objectives The aim of our study was to reveal whether inflammation affects BH4, IDO and GTP-CH1 (enzymatic) activity in JIA patients.
Methods Serum samples were collected of twenty-four JIA patients. In these samples, the concentrations of tryptophan, kynurenine, tyrosine, neopterin and phenylalanine were measured. An HPLC method with electrochemical detection was developed to quantify tryptophan, kynurenine and tyrosine. Neopterin and phenylalanine were quantified by ELISA. Kyn/trp ratio was measured as an index of IDO activity, while Phen/Tyr ratio was measured as an index of BH4 activity. Neopterin concentrations were used as an indirect measure of GTP-CH1 activity.
Results JIA patients with high disease activity showed higher levels of both neopterin and kynurenine, and a higher ratio of both Kyn/Trp and Phen/Tyr and lower tryptophan levels than clinically inactive patients.
Conclusions Altogether, these data support our hypothesis that inflammation increases the enzymatic activity of both IDO and GTP-CH1 and decreases the efficacy of the co-factor BH4. Further animal studies are needed to investigate whether inflammation-induced changes in these enzymatic pathways and co-factor lower the levels of the brain neurotransmitters dopamine and serotonin, and consequently produce sickness behaviour and fatigue.
Full text
https://www.mdpi.com/1424-8247/12/1/9/htm
2019
Abstract
Background Juvenile idiopathic arthritis (JIA) patients suffer from an inflammatory condition, resulting in painful joints. In addition, JIA patients often report symptoms of sickness behaviour, including depressive symptoms and fatigue. Recent animal studies suggest that proinflammatory cytokines produce sickness behaviour by increasing the activity of indoleamine-2,3-dioxygenase (IDO) and guanosinetriphosphate-cyclohydrolase-1 (GTP-CH1). Here it is hypothesised that inflammation in JIA patients affects the enzymatic activity of IDO and GTP-CH1 and the co-factor BH4. These compounds play a crucial role in the metabolism of the neurotransmitters serotonin and dopamine.
Objectives The aim of our study was to reveal whether inflammation affects BH4, IDO and GTP-CH1 (enzymatic) activity in JIA patients.
Methods Serum samples were collected of twenty-four JIA patients. In these samples, the concentrations of tryptophan, kynurenine, tyrosine, neopterin and phenylalanine were measured. An HPLC method with electrochemical detection was developed to quantify tryptophan, kynurenine and tyrosine. Neopterin and phenylalanine were quantified by ELISA. Kyn/trp ratio was measured as an index of IDO activity, while Phen/Tyr ratio was measured as an index of BH4 activity. Neopterin concentrations were used as an indirect measure of GTP-CH1 activity.
Results JIA patients with high disease activity showed higher levels of both neopterin and kynurenine, and a higher ratio of both Kyn/Trp and Phen/Tyr and lower tryptophan levels than clinically inactive patients.
Conclusions Altogether, these data support our hypothesis that inflammation increases the enzymatic activity of both IDO and GTP-CH1 and decreases the efficacy of the co-factor BH4. Further animal studies are needed to investigate whether inflammation-induced changes in these enzymatic pathways and co-factor lower the levels of the brain neurotransmitters dopamine and serotonin, and consequently produce sickness behaviour and fatigue.
Full text
https://www.mdpi.com/1424-8247/12/1/9/htm
Last edited: