This adenosine is certainly an important key.
Adenosine is metabolized into Inosine by deaminase enzyme, then catabolized into uric acid inside the cells.
Uric acid has neurologic anti oxidant properties, and was found to be inversely correlated with outcome in MS and ALS, so I would be interested if we can find the same in CFS/ME!
Inosine can actively binds to adenosine receptors A1 and A2A , so I guess the fact CFS/ME doctors gives inosine to their patients may be to compensate the adenosine deficiency.
I opened a thread about it here
https://forums.phoenixrising.me/ind...-anti-neurogenic-detrusor-overactivity.62212/
I didn't investigate the purinergic signaling /low adenosine link, but I found this study about Duchenne muscular dystrophy (below).
This study is very interesting because Allopurinol is blocking the Xanthine Oxidase, which is supposed to stop the Inosine catabolism into Uric acid (Allopurinol is a drug used to lower blood uric acid in gout patients).
Purine and carnitine metabolism in muscle of patients with Duchenne muscular dystrophy
Abstract
We determined levels of purines, purine metabolites, related enzymes and carnitine in muscle of 8 untreated Duchenne muscular dystrophy (DMD) patients, 12 allopurinol-treated DMD patients and 12 age-matched controls. Muscle of DMD patients was found to be deficient in ATP, ADP, adenylsuccinate, hypoxanthine, guanine and adenylsuccinate synthetase.
In allopurinol-treated DMD patients, mean total adenylate level was only three times less than in controls (versus 14 times less in untreated DMD patients).
Mean inosine monophosphate (IMP), adenine, adenosine, inosine, xanthine, guanine, guanosine and uric acid levels were higher in allopurinol-treated patients than in controls, while mean adenylsuccinate levels were higher than in untreated patients.
Allopurinol also restored acylcarnitine levels to normal and significantly increased free carnitine levels.
These findings strongly support the hypothesis that
Duchenne muscular dystrophy involves alterations leading to blockage of the IMP → purine pathway and that allopurinol treatment favours restoration of purine levels by this route.
Furthermore, our results suggest that the observed deficiencies in cell components unrelated to purine metabolism are long-term secondary effects.
However, another purine was one of the clearest and most consistent results: adenosine.
View attachment 24895
As you can see here adenosine levels were within a more narrow range and quite different on average between patients and controls. I haven't done p values on this but I guess I should.
View attachment 24897
Adenosine certainly has a range of interesting roles.
View attachment 24896
I'm personally always interested in vasodilation/vasocontraction problems (because of POTS, widespread problems with alcohol, the Fluge Mella NO patent, etc.). I think endothelial cells, being bloodflow facing immune signalling cells, are a perfect suspect that might decide to turn a local problem (lack of appropriate vascular tone) into a global one: an acute systemic immune response. Which could be a great explanation for PEM.
Adenosine is also tied up in metabolism, of course.
View attachment 24898
I'm certainly interested to hear if anyone can find any strong links from Adenosine to the puringeric signalling theory!
EDIT: this paper may be interesting:
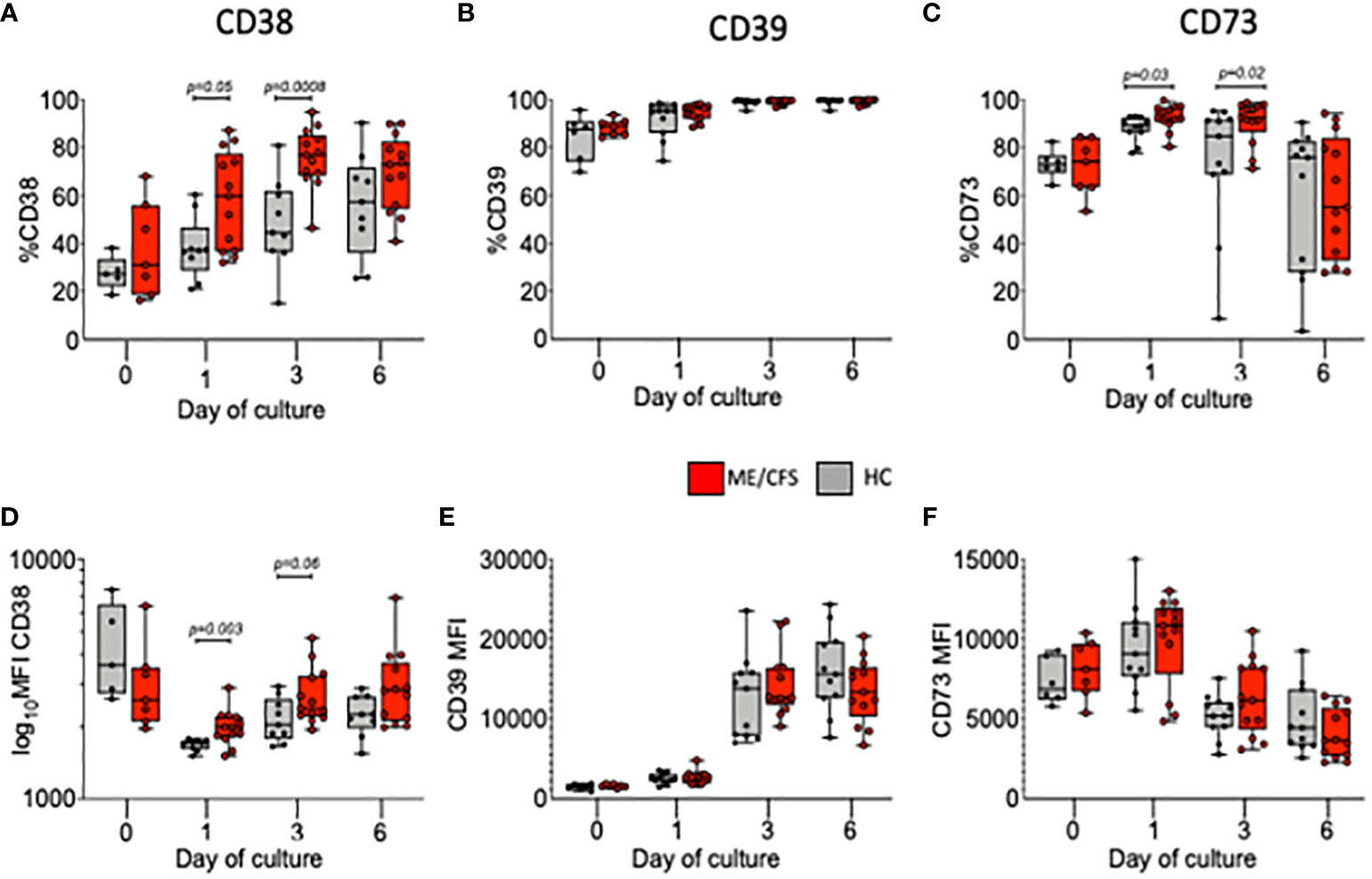
Extracellular Adenosine-Mediated Modulation of Regulatory T Cells
I've been reading the old original potato apyrase experiments which talk about ATP and the way it competitively interacts with ADP, AMP and adenosine. I wondered if this is the metabolic trap Phair was talking about - ATP getting in the way of other metabolic processes which require phosphorylation (such as ubiquinone), particularly at the PANX 1 channel. So as a little experiment, I started using glycyrrhetinic acid (licorice extract) as a PANX1 inhibitor - to slow down ATP into the extracellular space - and hence the p2x7 responsiveness. It's been a week (and I've started slow) I have less lactic acid and much more energy. I had a flare of what I think of as p2x3 responses - wide spread pain, trigeminal nerve issues, gut distention issues ect ect. I'm taking ALA for that but it takes awhile to take effect. All over, I'm feeling much better.