Differentiating ME/CFS from Primary Depressive and Anxiety Disorders without Co-Existing ME/CFS
[..]
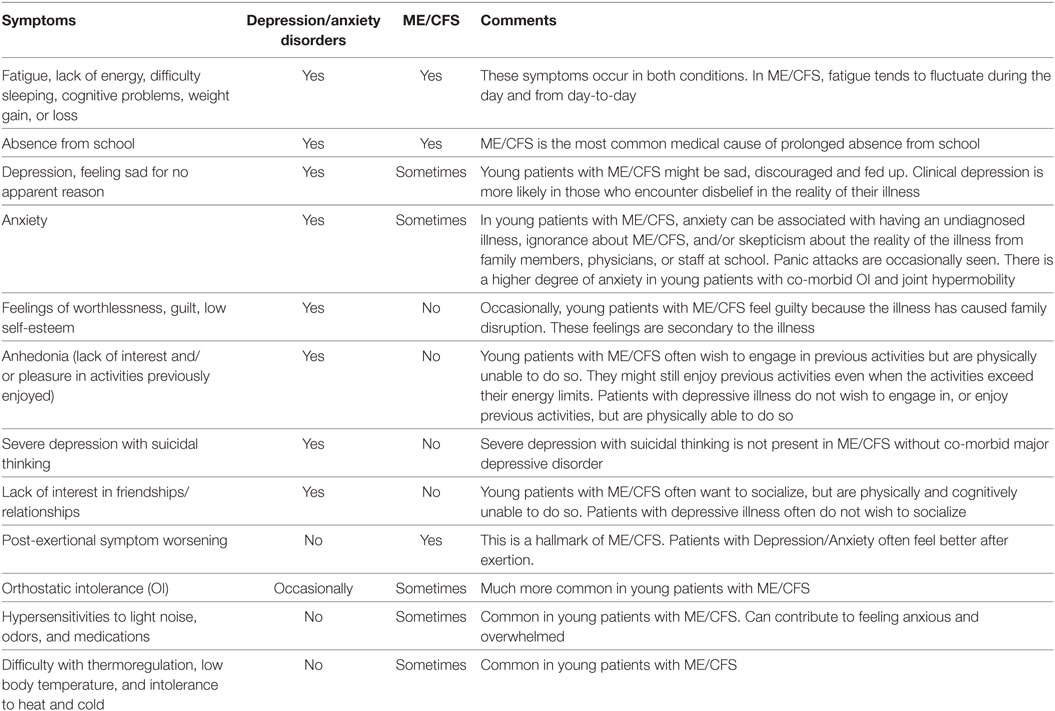
Some features distinguishing ME/CFS from primary psychiatric illnesses are shown in Table 5. In patients with ME/CFS, long-lasting post-exertional exacerbation of fatigue and other symptoms can follow mild exertion or even normal activity, whereas patients with major depression or anxiety often feel better after increased activity, exercise, or mental effort. OI, hypersensitivities to light, noise and medications and/or low body temperature, and intolerance to heat and cold are typical of ME/CFS, but not typical of psychiatric illnesses. Young women with ME/CFS often experience greater premenstrual mood lability.
Most teenagers with ME/CFS are highly motivated to recover and return to their previous lives. They generally have a strong desire to be more active, but cannot tolerate the necessary exertion. In contrast, patients with major depression do not have the desire to be more active but could be.
Adolescents with MDD show depressed mood, a sense of worthlessness or guilt, low self-esteem, loss of interest in socializing and in previously enjoyable circumstances (anhedonia), and a lack of interest in the future. Although these are typical symptoms of MDD, some young people with ME/CFS (but without co-morbid depressive illness) might also feel guilty because their illness has disrupted their family, and a parent might have had to give up work to care for them. They might also be reluctant to make plans to socialize, because they know from past experience that they might find themselves at the time of the event to be too ill to participate, have to cancel, and let down their friends. Anhedonia has not been reported in ME/CFS unless MDD was also present. Young people with ME/CFS often take much pleasure in previous activities, even if the activities exceed their energy reserves and cause subsequent symptom exacerbation.
In young people with MDD suicidal thoughts and suicide attempts can occur, more so in adolescents than in younger children. If suicidal thoughts are present a suicide evaluation should be done and referral to a child psychiatrist is often helpful. Suicidal thoughts are only seen in ME/CFS when MDD is also present.