Jesse2233
Senior Member
- Messages
- 1,942
- Location
- Southern California
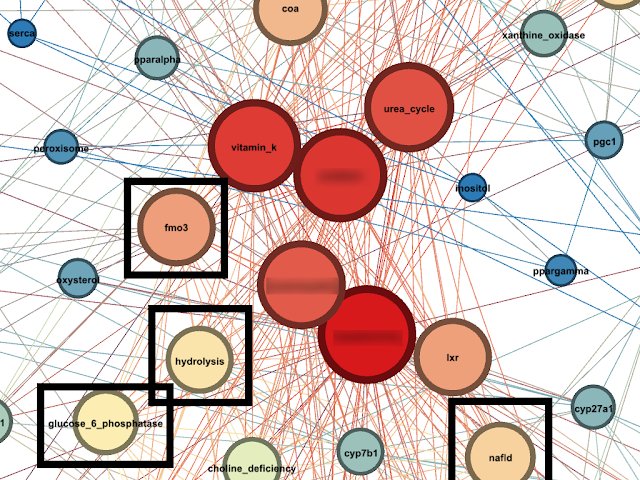
Good news! My friend is talking to Ron Davis on Friday about LXR

Welcome to Phoenix Rising!
Created in 2008, Phoenix Rising is the largest and oldest forum dedicated to furthering the understanding of, and finding treatments for, complex chronic illnesses such as chronic fatigue syndrome (ME/CFS), fibromyalgia, long COVID, postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome (MCAS), and allied diseases.
To become a member, simply click the Register button at the top right.
This is an interesting thread for me. My daughter has had skin reaction problems following chickenpox ( when under 5) and glandular fever /mono when 14. I never linked the skin problems/ allergies to liver function - our NHS was useless for this when she was small, treated it as eczema that she would grow out of, prescribed multiple hydrocortisone creams and we eventually saw a naturopath who determined an intolerance for bleached food. Cut this out for a while and the skin issues receded ( eat too much bleached flour/sugar and it comes back).One example is methylation problems.
Thanks @mariovitali Can you advise what is this please?@anni66 please consider taking a Fibroscan test
I had low albumin. Never took those drugsI had low albumin. (Which the doctor said was fine
.) So that is now an alarming number + 1. Has anyone polled the patients here to look for trends like this?
Many thanks for this - we have a GP appointment next week so I will find more info to back up request.Fibroscan is an alternative to Liver Biopsy. Note that even if Liver enzymes are normal, you may have advanced Liver Disease.
You can ask your GP although having lived in the UK i am quite certain that a GP will only approve a Fibroscan in case of elevated Liver Enzymes only.
Here is more info :
http://www.fibroscan.com/en/products
Thanks, i will try@anni66
No problem. I also suggest you test for Transketolase, Albumin, Zinc, Copper, Ceruloplasmin and Total Bile Acids..i know these are difficult to get but i am writing them in any case.
@Inester7
How did you get ME/CFS?
- The protein encoded by this gene is a transcriptional coactivator that regulates the genes involved in energy metabolism. This protein interacts with PPARgamma, which permits the interaction of this protein with multiple transcription factors. This protein can interact with, and regulate the activities of, cAMP response element binding protein (CREB) and nuclear respiratory factors (NRFs). It provides a direct link between external physiological stimuli and the regulation of mitochondrial biogenesis, and is a major factor that regulates muscle fiber type determination. This protein may be also involved in controlling blood pressure, regulating cellular cholesterol homoeostasis, and the development of obesity. [provided by RefSeq, Jul 2008]
Medications can directly inhibit mtDNA transcription of ETC complexes, damage through other mechanisms ETC components, and inhibit enzymes required for any of the steps of glycolysis and b-oxidation. Indirectly, medications may damage mitochondrial via the production of free radicals, by decreasing endogenous antioxidants such as glutathione and by depleting the body of nutrients required for the creation or proper function of mitochondrial enzymes or ETC complexes. Damage to mitochondria may explain the side effects of many medication
Ox-phos is the major cellular energy-producing pathway. Energy, in the form of ATP, is produced in the mitochondria through a series of reactions in which electrons liberated from the reducing substrates nicotine adenine dinucleotide (NADH) and flavin adenine dinucleotide (FADH) are delivered to O2 via a chain of respiratory proton (H+) pumps [8
Compounding the problem, once a mitochondrion is damaged, mitochondrial function can be further compromised by increasing the cellular requirements for energy repair proc- esses [9]. Mitochondrial dysfunction can result in a feed- forward process, whereby mitochondrial damage causes additional damage