Hi there,
I'm looking for some wisdom regarding Chronic Histamine Intol, affecting especially the central nervous system and causing food triggered migraines.
I've been suffering from such for the last 7 years and no regular doctor could shed a light on the way of the solution to my problem.
My symptoms are as follows:
Upon ingestion of most food groups, like any type of fruit, gluten and no gluten foods (bread, etc), chocolate, tea, soft drinks, sweeteners, milk, yogurts, Honey, caffeine, Kinua, grape juice and wine, etc....a metallic taste develops on the tip of my tong. Following, I develop black eyes (vasodilation effect) , asymptomatic hypotension (80 x 50 mmHg), and 6 to 8 hours later, a bad classic migraine.
Symptoms worsen along the day and build up the more food I eat. It seems to be dose dependant.
If I stay away from a particular food, like for instance a Coke, the reaction is milder, and as long as I keep exposing myself to the same drink, I tend to develop a stronger and faster reaction.
Eventually, if I insist in the same food, I develop a skin eczematous itchy rash that becomes elevated and warm.
Food that don't cause any reactions are meet, fish, chicken, rice, beans, salad, tomatoes, regular cheese.
I've been to a ton of tests and none have helped. Gluten intolerance was ruled out and even a biopsy was done to confirm that.
I've tried many migraine prophilactic medications but they did not help. The only medication that helped a little was Flunarizine, a Calcium channel blocker. After using it for a year in a very low dose, eventually It made me very tired and upon stopping it, the symptoms became worse again.
My symptoms are relieved by Triptans and I've been taking one of those every night and the following day, the same story starts again.
I've also developed a chronic constipation as it doesn't seem to be an easy way to help my bowels function properly. Recently I've started taking some Chia in the hopes it helps.
Chronic Histamine Intolerance affecting primarily the SNC seems to be a fairly reasonable diagnosis.
Is there I way to fix this.
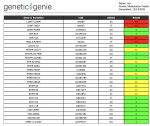
I was thinking, histamine metabolizing probiotics, diaminooxidase, SAM-e to help my HMNT.
Can somebody let me know their thoughts?